Paleo vs. Keto: What's the Difference?

Peas in a Pod, or Beets vs. Broccoli
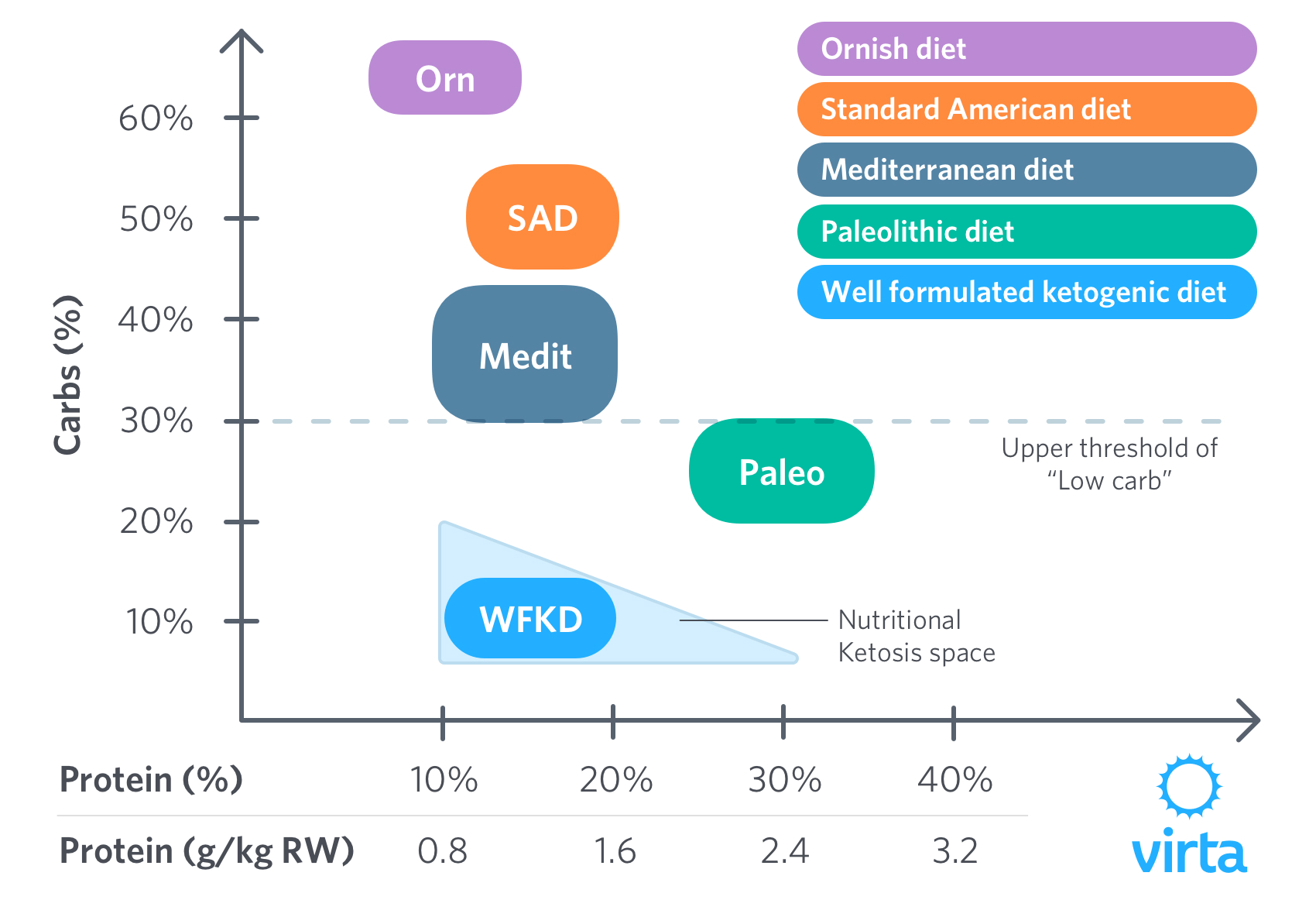
There are a lot of similarities between Paleolithic (Paleo) and ketogenic diets (KD), particularly when compared to the now discredited ‘Standard American’ low fat, high carbohydrate diet. As a result, people may reasonably assume that all low carb diets are pretty much equal in their nutrient contents and physiological benefits. Unfortunately, this is far from the truth, and the resulting confusion has distracted us from fully understanding how best to apply carbohydrate-restriction to improve individual well-being and function.
The similarities between Paleo and keto cluster around what they exclude: all grains and grain products (refined and unrefined), peas and beans, and refined sugars. In addition, the paleo diet excludes all dairy (milk, cream, and cheese), whereas the ketogenic diet allows butter, full fat cream and natural cheeses.
The differences between the Paleo diet and KD are many, including:
- Range of foods allowed
- Recommended amounts of protein
- Amounts and sources of carbohydrates allowed or recommended
- Type, quality, and quantity of science supporting diet safety and efficacy
- Most importantly, the source and consistency of fuel to supply brain energy needs – specifically the availability of ketones at adequate levels to replace glucose as the brain’s primary fuel

If you are keeping score, there are two categories of food that you lose on a ketogenic diet (high sugar fruits and starchy vegetables) vs one that you lose on the Paleo diet (full-fat dairy).
But if you think of these foods in terms of taste and how much they satisfy your hunger, giving up cheese, butter and cream (not to mention ice cream) is a major ‘minus’ for the Paleo diet. Think of creamed spinach, mushrooms sautéed in butter, or oven-roasted cauliflower sprinkled with parmesan cheese.
Macronutrients in Perspective
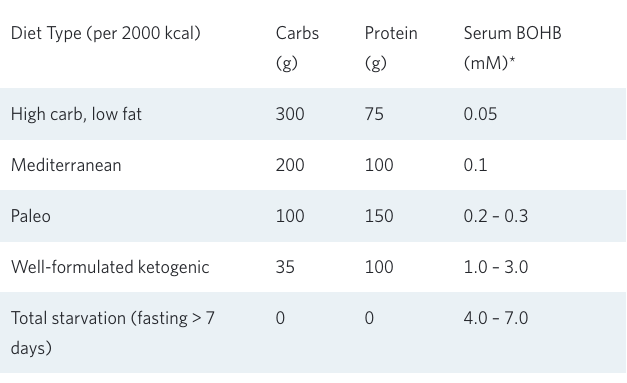
This diagram points out the similarities between ketogenic and Paleo diets, especially when compared to the now discredited low fat diets of the past. But clearly the Paleo and well-formulated ketogenic diets nonetheless are different, with little overlap in their respective compositions.
The Historical Origins of Paleo and Ketogenic Diets
The Paleolithic diet is based upon the observation that for hundreds of thousands of years, our human ancestors were hunter-gatherers. Access to agricultural grains, tubers, and beans—domesticated within the last 10,000 years—are recent events in human evolutionary history, as is getting milk from animals. Advocates of the Paleo diet contend that grains, beans and dairy can irritate the human digestive tract and don’t belong in a healthy diet (Cordain 2005). They report that eliminating these foods can eliminate many inflammatory conditions and improve athletic performance.
The ketogenic diet has been around since our ancestors began to hunt, and particularly in the million or so years since they began to move out of the tropics. However to achieve nutritional ketosis, consumption of fruit, roots, and wild grains had to be very limited; and in addition, their choice of what to hunt and what to eat from their prey needed to emphasize higher fat and less lean meat (Stefansson 1946). Learning these lessons allowed humans to extend their range into higher latitudes and high altitudes (e.g., the Inuit and the Mongols) where access to gathered carbs was limited or nonexistent.
This perspective raises two questions. First, is the ability to tolerate nutritional ketosis limited to humans whose ancestors evolved to live for thousands of years on a ketogenic diet? Briefly, the ability to make and use ketones in place of blood glucose allows humans to go without food for periods of weeks up to a few months when necessary for survival, which has benefited all human racial groups and cultures. And human infants who are breastfed are in continuous ketosis for the first week of breastfeeding, and then intermittently so for the next 6 months (Cahill memoire, 2006). Babies’ brains love ketones.
Which leads to the second question. Given access to dietary carbs, why would an individual or a whole culture voluntarily choose to avoid carbohydrate-rich fruit and vegetables (e.g., the Masai in the Great Rift Valley and the nomadic buffalo hunters of the US Great Plains)? There are many potential answers to this question, but here are two—portability and nutritional ketosis. For nomadic people, the weight of their food matters if they have to carry it, and fat (whether butter or pemmican) weighs less than half as much per calorie as fully dried grain or beans. As for nutritional ketosis, it is likely that some cultures made the empirical discovery that they felt better and functioned better when they avoided excess carbs and ate protein in moderation (Orr JB, 1931; Stefansson 1946; Schwatka 1965), and recent scientific discoveries have helped explain why this occurs (Forsythe 2008; Schimazu 2013; Newman 2014; Volek 2016).
Nutritional Ketosis
Thus the major metabolic difference between Paleo and KD is encompassed in the phrase ‘nutritional ketosis’. By definition, a ‘ketogenic diet’ allows your body to be in nutritional ketosis, whereas a Paleo diet seems to be purposefully designed to prevent it.
Why is that important? The KD provides a natural and sustained fuel supply to your brain, whereas the Paleo diet requires that you consume a steady supply of just enough carbs from fruits and starchy vegetables to feed your brain the 600 Calories it needs day-in and day-out to maintain its basic functions.
It is a common assertion among Paleo advocates that the high sugar fruit and starchy vegetables are absolutely necessary for normal brain function and metabolic health. In one sense, they are partially correct. If you eat enough carbs (and/or excess protein) to prevent the body from making adequate ketones to nourish your brain, then you do have to regularly eat enough carbs and protein to supply it with 600 Calories of glucose per day. Thus the Paleo edict that at least 20% of your dietary energy needs to come from carbs (e.g., 400 kcal out of a 2000 kcal diet, with the other 200 kcal coming from gluconeogenesis). But this is true only if you are not in nutritional ketosis.
Keto-adaptation
The other important fact necessary to understand the ‘Paleo-fed brain’ vs the ‘ketone-fed brain’ is that once dietary carbs fall below the minimum level necessary to provide glucose to the brain, the body initially struggles to maintain fuel flow to the brain. Among other things, the liver has to work overtime to convert protein into glucose, often at the cost of muscle loss. And although the liver promptly accelerates ketone (beta-hydroxybutyrate, aka BOHB) production from fat, it takes the body a few weeks to channel these ketones as the brain’s primary fuel. During this hiatus in the switch from glucose to ketones, aka BOHB, most people feel a lag in energy plus increased appetite and food cravings.
But once through this phase, called keto-adaption, the brain is freed from its dependence on the glucose it derives from dietary carbohydrates, nourished instead by a steady and unwavering supply of BOHB from the liver. Cravings and appetite subside, and ‘hitting the wall’ during exercise no longer occurs. However, this smooth energy flow can be promptly reversed by eating either too much carbs or even too much protein.
These carb/protein intake thresholds below which nutritional ketosis occurs vary from person to person, but the standard Paleo energy prescription (30% protein, 20% carbs, 50% fat) is pretty much guaranteed to prevent nutritional ketosis. For most people to enter and maintain the keto-adapted state, dietary carbs need to stay under 5–10% of daily energy needs. This explains why you can’t have high sugar fruit and starchy vegetables and still be in nutritional ketosis. Protein needs to be eaten in moderation—in the range of 15–20% of daily energy—because eating more than this starts to drive down your ketone level.
In contrast to the common misconception that all low carb diets are necessarily high in protein, a well-formulated ketogenic diet requires that protein intake be kept in this moderate range. Given that carbs (5–10%) and protein (15–20%) together add up to about 25% of your daily energy intake, this means that the other 75% of your daily energy has to come from fat. If you need to lose some weight, initially some of this 75% can come from body fat stores, but once at your desired body weight, all of the fat that you need for daily energy necessarily comes from your diet.
Inflammation and Recovery
It is a common observation that when people (be they athletes or not) make the switch from Paleo to a well-formulated ketogenic diet, they notice a number of positive changes. These typically include:
- Nagging stomach and bowel issues go away (a common side effect of a high protein diet)
- An increased and more sustained energy level
- Less general aches and pains in muscles and joints
- More rapid recovery after exercise (be it an evening of dancing or running a marathon)
For the last few decades, we have noticed that a well-formulated ketogenic diet reduces inflammation levels in our research subjects, but we didn’t know why (Forsythe, 2008). Recently, a team of scientists in San Francisco discovered that nutritional ketosis (blood BOHB between 1–3 mM) triggers a powerful switch that turns on the body’s defenses against oxidative stress, also known as free radicals—a major stimulus for inflammation (Schimazu 2013). So now we know that BOHB is much more than an excellent fuel for the brain. When you cut your carbs and moderate your protein on a well-formulated ketogenic diet, the naturally occurring BOHB levels in your body help protect it from the stresses (i.e., oxidative stress and inflammation) of daily life and the damage caused by exercise. It is also very likely that circulating BOHB benefits intestinal function in two ways; both as a preferred fuel for the cells that line the inside of the colon, and also as a specific signal to those cells' genes to turn down inflammation pathways (Youm 2015).
Dietary Factors Affecting Gut Health
This is a very complex topic deserving of its own chapter or post. Important issues relevant to the current discussion are fiber, microbiome, gut irritants, lactose, and ketones. Both a Paleo and a ketogenic diet provide enough vegetables, nuts, seeds, and berry (fruit) to nourish a healthy microbiome. Both remove all grains that contain gluten, although gluten-induced celiac disease is far less prevalent (1–4%, depending upon ethnic origin) than popularly assumed. Lactose intolerance affects about half of the adult population in the US. But because this problem is dose-dependent and the high-fat dairy options offered with a well-formulated ketogenic diet contain very little lactose and whey, the complete avoidance of dairy products with the Paleo diet offers little added benefit over the KD. Irritable bowel syndrome, on the other hand, is an inflammatory disorder affecting about 10% of the population worldwide. BOHB is both a preferred fuel and an anti-inflammatory signal for the cells lining the colon. Between these two, they explain why irritable bowel syndrome is more commonly resolved with a ketogenic diet (Austin 2009). In a nutshell, on the topic of gut health, Paleo has many benefits, with an advantage for those uncommon cases of true milk protein allergy. The KD is almost as good as Paleo in dealing with food intolerance and allergy-induced symptoms, but it delivers superior results when it comes to optimizing gut fuel and inflammation.
Why this isn’t happening in the mainstream
We are occasionally asked: “If this story is so clear and compelling, why isn’t it more generally known and accepted?”
Perhaps it is because, like quitting smoking, it’s initially challenging to give up a life-long habit, not to mention overcoming carbohydrate cravings during the keto-adaptation process. Or perhaps it’s because the words ‘ketone’ and ‘ketogenic’ strike fear into the hearts of most classically-trained doctors and dietitians. This is due to the fact that the only training most doctors, dietitians, and nutritionists receive on ketones is about the dangers of diabetic keto-acidosis, a dangerous condition that occurs when ketones are in the range of 10–25 mM—10-fold higher than with a well-formulated ketogenic diet. Thus it should come as no surprise that much of this knee-jerk pushback against nutritional ketosis has trickled down to coaches and trainers who represent the front-line of nutrition counseling. As a result, there are many popular diets said to derive the benefits of carbohydrate restriction—think Paleo or intermittent fasting—without the presumed ‘risks’ associated with a ketogenic diet.
Research—Nutrition’s ‘Final Frontier’
Most of us used to assume that our government’s dietary advice was based upon carefully done and comprehensive research. In recent years, however, courageous investigative journalists like Gary Taubes and Nina Teicholz have challenged the very foundations of the US Dietary Guidelines. Nonetheless, in reality, what we are told is healthy to eat is still mostly determined by:
- Agricultural industry lobbyists who are paid to promote grains, sugar, refined carbs, and highly processed foods
- Cultural norms and habits (the French eat bread, Germans eat potatoes, Italians pasta, Chinese rice, etc). Americans? We have been encouraged to eat all of the above.
- Politically astute nutrition scientists who figure out how to do studies that support the consensus (ie, what the ag-industry lobbyists and cultural norms dictate). Simply put, it is easier to go with the flow of Gatorade and orange juice than to go against the grain.
Within this context of misdirected mainstream dietary advice, the Paleolithic and ketogenic diet strategies look like two peas in a pod. That said, however, in the last decade there has been a surge in scientific attention that is specific to nutritional ketosis. Rather than being equally divided between these two similar low carbohydrate paradigms, most of the science is on the side of nutritional ketosis. It is informative to compare the simple volume of published scientific literature for ‘paleolithic diet’ and ‘ketogenic diet’ using PubMed. As of November 2017, the former registers 192 publications, whereas the latter comes in at 2,143.
Thus the predominant topic for research in the low carb arena is focused on nutritional ketosis (including much from scientists who have recently freed themselves from the mainstream consensus). Hopefully more scientists and journal editors will do what we expect scientists to do—go where these data lead and advocate evidence-based medicine.
Paleo—One Step in the Right Direction
Clearly the high carb, low fat paradigm promoted by the mainstream nutrition consensus over the last 5 decades has been the primary cause of our current epidemic of obesity and diabetes.
Against this failed hypothesis, the Paleo diet represents a positive force for change. Eliminating sugar, refined starch, and processed foods from our diet will begin to turn back our epidemics of obesity and diabetes. And from a marketing perspective, it is easier to sell the public on a pretty good thing that they are willing to embrace rather than a great thing that goes against deeply held beliefs. But particularly for people with underlying insulin resistance and diseases caused by inflammation, optimizing fuel flow, supplying the brain with adequate energy, and driving down oxidative stress and inflammation requires another step beyond Paleo—cutting out the high sugar fruits and starchy vegetables and embracing nutritional ketosis.
Have more questions about nutritional ketosis? Check out our FAQ by Dr. Steve Phinney and the Virta team.
The information we provide at virtahealth.com and blog.virtahealth.com is not medical advice, nor is it intended to replace a consultation with a medical professional. Please inform your physician of any changes you make to your diet or lifestyle and discuss these changes with them. If you have questions or concerns about any medical conditions you may have, please contact your physician.
This blog is intended for informational purposes only and is not meant to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition or any advice relating to your health. View full disclaimer
Are you living with type 2 diabetes, prediabetes, or unwanted weight?

- Austin GL, Christine B.Dalton CB, Hu Y, Morris CB, Hankins J, Weinland SR, Westman EC, Yancy WS Jr, Drossman DA. A Very Low-Carbohydrate Diet Improves Symptoms and Quality of Life in Diarrhea-Predominant Irritable Bowel Syndrome. Clin Gastro Hep. 2009; 7:706-708.
- Cahill GF Jr. Fuel Metabolism in Starvation. Annu. Rev. Nutr. 2006; 26:1–22 doi: 10.1146/annurev.nutr.26.061505.111258
- Cordain L. The Paleo Diet. 2005; Wylie & Sons, NY, NY.
- Forsythe CE, Phinney SD, Fernandez ML, Quann EE, Wood RJ, Bibus DM, Kraemer WJ, Feinman RD, Volek JS. Comparison of low fat and low carbohydrate diets on circulating fatty acid composition and markers of inflammation. Lipids. 2008; 43:65-77.
- Newman JC, Verdin E. β-hydroxybutyrate: much more than a metabolite. Diabetes Research and Clinical Practice. 2014; 106:173-181.
- Orr JB, Gilks JL. The physique and health of two African Tribes. Medical Research Council, 1931; London.
- Shimazu T, Hirschey MD, Newman J, He W, Shirakawa K, Le Moan N, Grueter CA, Lim H, Saunders LR, Stevens RD, Newgard CB, Farese RV Jr, de Cabo R, Ulrich S, Akassoglou K, Verdin E. Suppression of oxidative stress by β-hydroxybutyrate, an endogenous histone deacetylase inhibitor. Science. 2013; 339:211-4.
- Schwatka F. The Long Arctic Search. The Marine Historical Assoc. 1965; Mystic, CT.
- Stefansson V. Not by Bread Alone. 1946; McMillan NY, NY. pp 136-142.
- Volek JS, Freidenreich DJ, Saenz C, Kunces LJ, Creighton BC, Bartley JM, Davitt PM, Munoz CX, Anderson JM, Maresh CM, Lee EC, Schuenke MD, Aerni G, Kraemer WJ, Phinney SD. Metabolic characteristics of keto-adapted ultra-endurance runners. Metabolism. 2016; 65:100-10.
- Youm YH, Nguyen KY, Grant RW, Goldberg EL, Bodogai M, Kim D, D'Agostino D, Planavsky N, Lupfer C, Kanneganti TD, Kang S, Horvath TL, Fahmy TM, Crawford PA, Biragyn A, Alnemri E, Dixit VD. The ketone metabolite β-hydroxybutyrate blocks NLRP3 inflammasome-mediated inflammatory disease. Nat Med. 2015; 21:263-9.