
Type 2 Diabetes
An evidence-based guide to type 2 diabetes
and your treatment and reversal options.
Type 2 diabetes is a national health crisis
If you are an adult living in the United States, you are now more likely than not to either have type 2 diabetes or be on your way to developing it. 14.3% of US adults have type 2 diabetes, and 38.0% of US adults have prediabetes, meaning that 52.3% of the adult population in the US is suffering from metabolic disease.
in the US is suffering
from metabolic disease

Nearly 4 in 10 US adults
have prediabetes

1 in 7 US adults have
type 2 diabetes

What is type 2 diabetes?
Prediabetes is used to describe an earlier stage of insulin resistance where blood sugar that is elevated above normal, but not high enough to be called type 2 diabetes. An American Diabetes Association expert panel estimated that up to 70% of individuals with prediabetes will eventually develop diabetes.1 But because prediabetes has few obvious symptoms, 90% of people with prediabetes don’t know they have it.2
At the most basic level, diabetes is a term used to describe a group of diseases that result in high blood sugar. Type 2 diabetes, (also called diabetes mellitus type 2) represents about 95% of what is generically called “diabetes.” Early in its course, type 2 diabetes is characterized by the combination of very high insulin levels and high blood sugar. In a person without diabetes, such high insulin levels would rapidly reduce blood sugar to normal, but in type 2 diabetes the body becomes resistant to the action of insulin (also known as ‘insulin resistance’), making blood glucose levels hard to control with insulin and other standard medications.
What are the symptoms of type 2 diabetes?

Type 2 diabetes symptoms include:
- Fatigue
- Increased thirst and dry mouth
- Increased urination
- Frequent vaginal or urinary infections
- Erectile dysfunction
- Increased hunger
- Neuropathy (numbness, tingling in feet and hands)
- Blurred vision
- Slow-healing sores or frequent infections
- Weight gain
Prediabetes symptoms include:
- Feeling tired and hungry all the time
- Poor sleep
- Difficulty focusing
- Neuropathy (numbness, tingling in feet and hands)1
- Neck skin darkens
- Developing many small skin tags
- Weight gain
How do you know if you have type 2 diabetes?
Type 2 diabetes symptoms include:
- Fasting blood sugar of 126 mg/dL or higher on two separate occasions
- HbA1c of 6.5% or higher
- An oral glucose tolerance test that shows a blood sugar of 200 mg/dL or higher after 2 hours
Prediabetes symptoms include:
- Fasting blood sugar of 100–125 mg/dL on two separate occasions
- HbA1c of 5.7–6.4%
- An oral glucose tolerance test that shows a blood sugar of 140 mg/dL or above after 2 hours.
Where does high blood sugar come from?
Everyone has glucose, a type of sugar, in their blood at all times. Sugar is a source of energy—it can supply the cells in your body with the energy they need to perform critical functions, ranging from powering your brain to fueling your muscles during high intensity exercise.
When eating a standard American diet, most of the sugar in your blood comes from a particular food source—carbohydrates, also called carbs. Starchy foods such as bread, potatoes, pasta, rice, baked goods and table sugar are commonly referred to as carbs, but “carbs” actually refers to a type of molecule inside these foods.
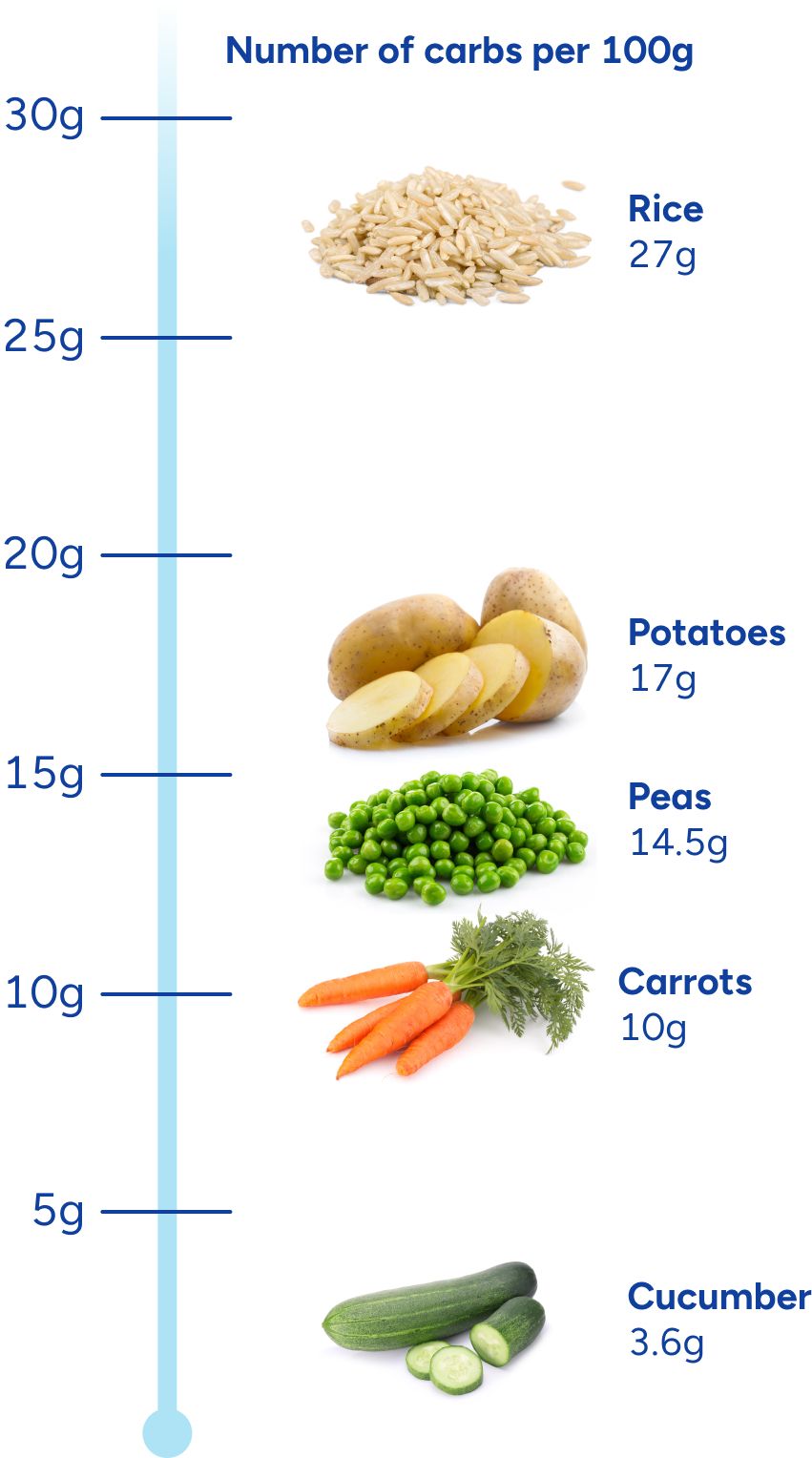
There are also high levels of carbohydrate molecules in most fruit, fruit juices, sugary beverages, and starchy vegetables such as carrots, yams, corn, dried beans, and peas. In contrast, there are low levels of carbohydrate molecules in non-starchy vegetables such as leafy greens, cucumbers, green beans, peppers, and broccoli.
For example, the amount of carbohydrates in 100 grams of the following foods varies significantly: rice (27g); potatoes (17g); peas (14.5g); carrots (10g); cucumber (3.6g).
Carbohydrate molecules like starch are just chains of sugar units, but your body can’t absorb the long chains. During digestion, your body breaks down these chains of sugar units into pieces that it can absorb. These pieces are sugar molecules, most of which are glucose (blood sugar). That’s why when you eat foods containing carbs, it raises your blood glucose—you are absorbing the sugar directly into your bloodstream.
The Role of Insulin
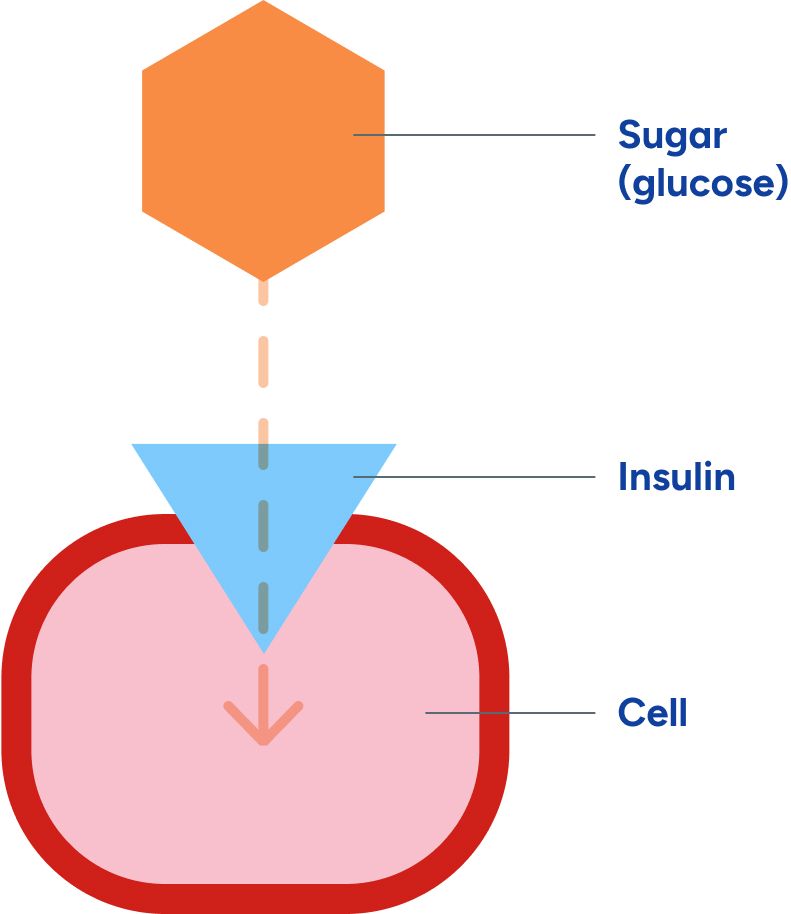
Once this sugar has been absorbed into your bloodstream, it still has to travel a bit farther—in order to be used for energy, the sugar circulating in your blood needs to get inside your cells. That’s where insulin comes into play. Insulin is a chemical messenger produced by your body — a hormone that also helps with growth, fat storage and energy use. Insulin helps move the sugar from out of your blood into your cells, so that it can be used for energy.
Eating carbohydrates results in an increase in blood sugar. Insulin is needed to keep that increase to a minimum. So each time you eat carbohydrates and your blood sugar rises, your body then releases insulin in order to move the sugar into the cells. But if for some reason the body stops responding to the signal of insulin, then the sugar cannot adequately enter your cells, and so it stays in your blood. This causes high blood sugar.
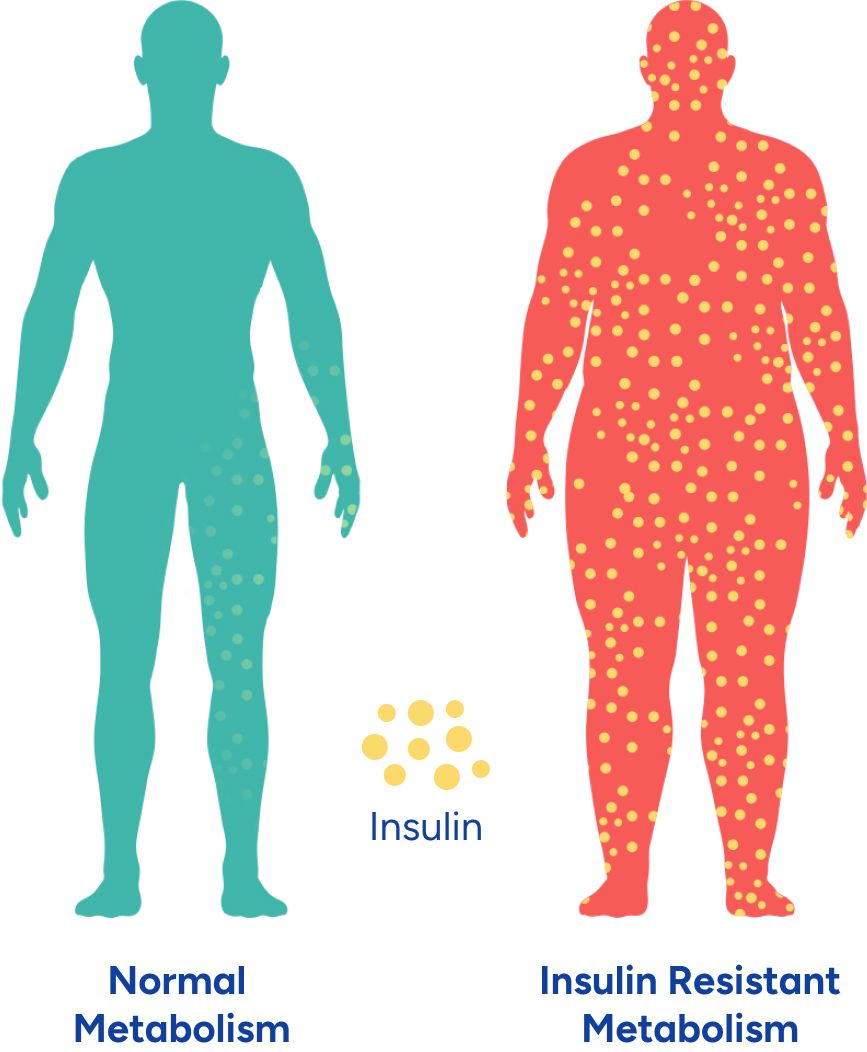
Insulin Resistance
Type 2 diabetes is caused by insulin resistance, a condition in which cells stop responding properly to the signal of insulin. While the root causes of insulin resistance are not fully understood, the bottom line is that adding more insulin does not fix the underlying problem. While your insulin will still rise in response to eating carbohydrates, since your cells are not responding to its signal, your blood sugar cannot be moved into cells effectively. This leaves you with both high blood sugar and high insulin.
Over many years, trying to compensate for the chronically elevated blood sugar requires that your body pumps out insulin at a much higher rate than it’s supposed to. Once we reach adulthood, our ability to grow new insulin-producing cells in the pancreas is limited3, so when insulin production is over-stressed, these cells are lost and not replaced. That’s why long-term type-2 diabetes can lead to a loss of the ability to produce much insulin on your own. When you lose most of your ability to produce insulin on your own, that is called pancreatic burnout. At this stage in the progression of type 2 diabetes, injected insulin becomes necessary to replace your body’s dwindling supply.
Insulin resistance is associated with many health problems in addition to type 2 diabetes and prediabetes, including metabolic syndrome, polycystic ovary syndrome (PCOS), atherosclerotic heart disease, fatty liver disease, and more.4-7
High blood sugar is a sign of carbohydrate intolerance
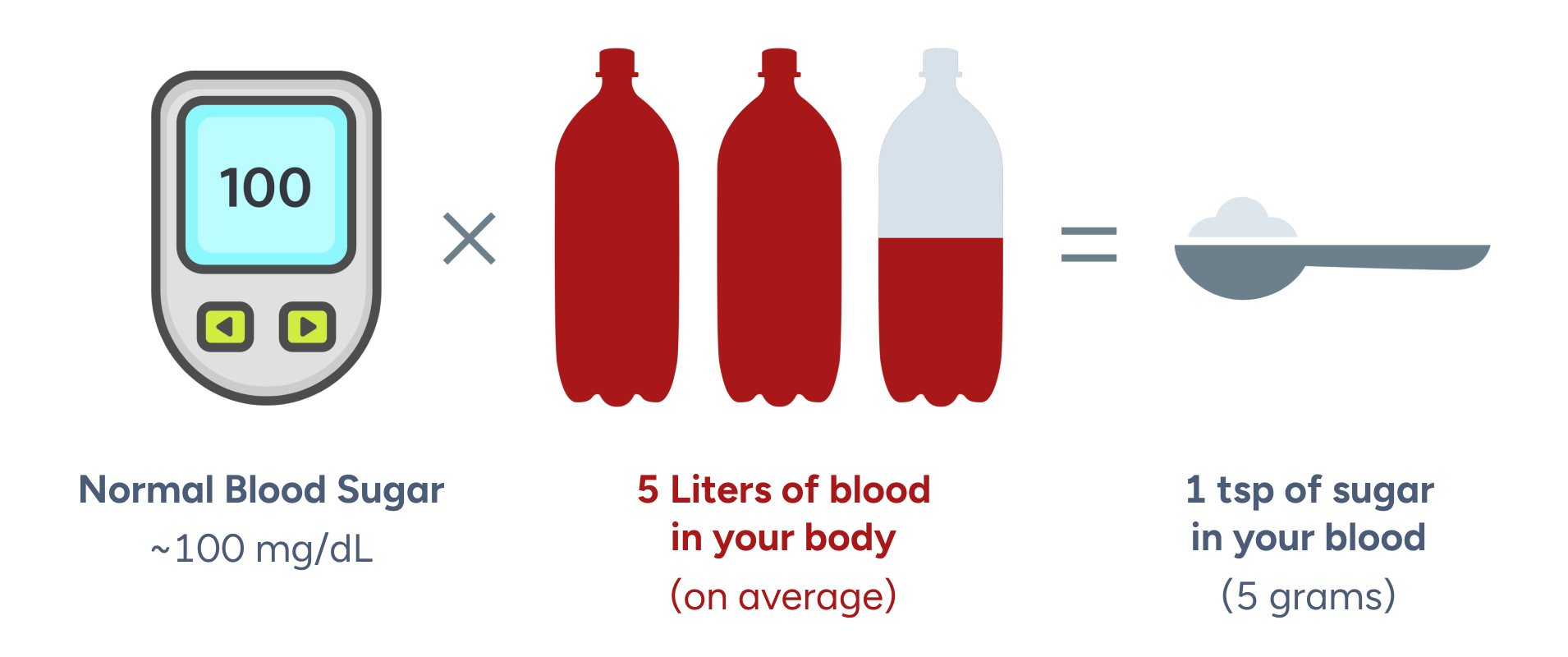
Normal blood sugar is generally considered to be a fasting blood sugar under 100 mg/dL, or 70-140 mg/dL 2 hours after a meal. In the 5 liters of total blood in your body (on average), this is equivalent to about 1 teaspoon of sugar circulating in your blood.
Your body tries to keep your blood sugar in this range because high blood sugar can cause serious damage to your blood vessels and organs, leading to some of the terrible outcomes associated with type 2 diabetes like blindness, kidney failure, and amputations. So when your blood sugar starts to climb above this normal range, your body will markedly increase its insulin secretion to move the additional sugar out of your blood and into your cells.
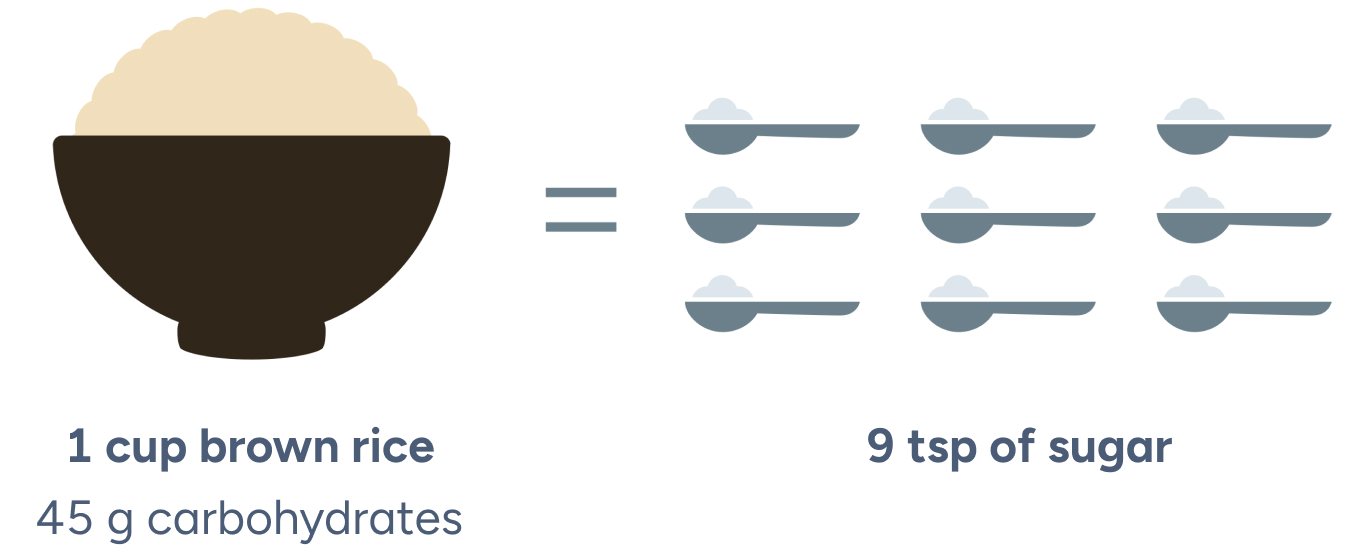
When you eat a food that has a lot of carbs in it, like a cup of white (or even brown) rice, your blood sugar will climb rapidly. This occurs because the carbs in the rice are rapidly converted to sugar. In fact, 1 cup of rice has about 45 grams of carbs in it, which means about 9 teaspoons of sugar is going to be absorbed into a system that tries to stay at about 1 teaspoon of sugar at all times.
For some people, getting their blood sugar down to normal after a high carb meal is relatively easy. They are very sensitive to the signal of insulin, meaning their body can efficiently move the sugar of their blood and into their cells. This can be thought of as a high carbohydrate tolerance, as they can respond to eating a lot of carbs without having blood sugar problems.
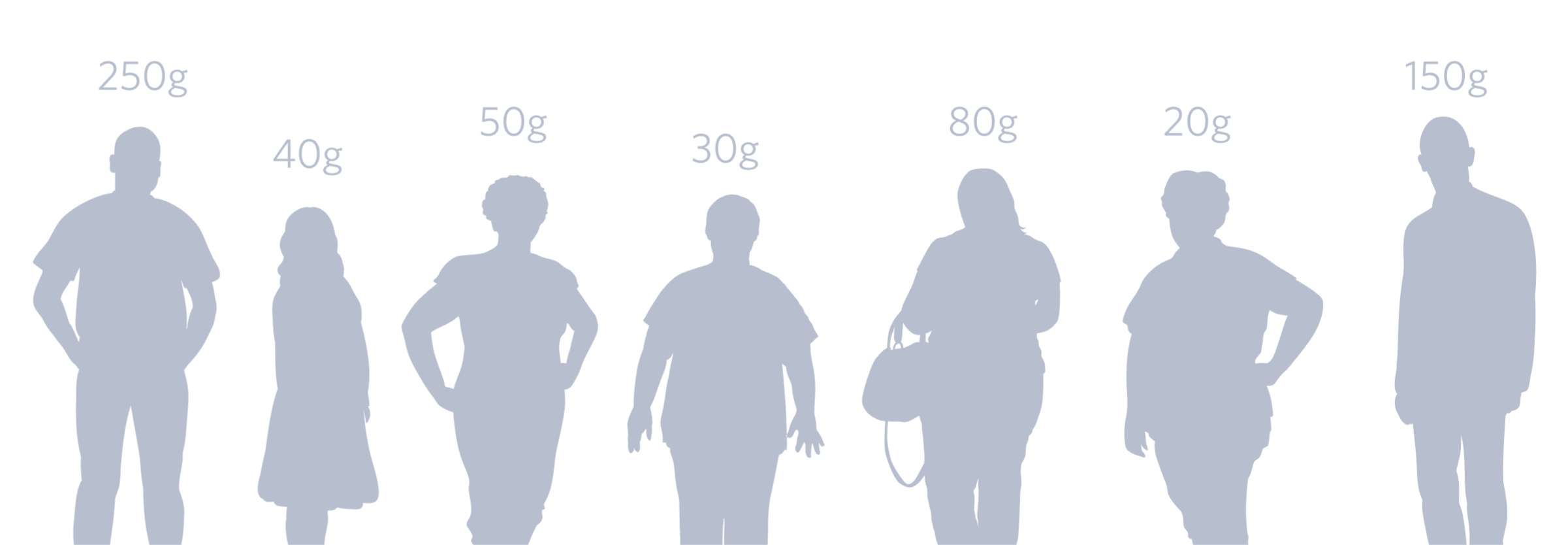
But for people with type 2 diabetes or prediabetes, getting their blood sugar down to a normal level after a high carb meal is extremely difficult. These people are resistant to the signal of insulin, meaning their body is struggling to move all of that sugar out of their blood and into their cells, leaving their blood sugar high. This can be thought of as low carbohydrate tolerance or carbohydrate intolerance. For many people, particularly those with a family history of diabetes, years of exposure to a standard diet (typically providing the equivalent of 10–15 teaspoons of sugar per meal) leads to increasing insulin resistance and carbohydrate intolerance.
If you imagine the cells as tiny storage lockers, then insulin is the key that opens the locker doors.

When you have type 2 diabetes, you are already struggling with chronically elevated blood sugar due to insulin resistance—so you are already carbohydrate intolerant. In someone who is carbohydrate intolerant, a much higher level of insulin is needed to reduce their blood sugar to a normal level than in someone who is not carbohydrate intolerant.
So, carbohydrate intolerance means that for an equal amount of carbohydrates consumed, the insulin needed to keep blood sugar from rising is much greater.
Everyone has a unique carbohydrate tolerance
Type 2 Diabetes Isn’t Just a Disease of High Blood Sugar—Inflammation Matters Too
While diabetes is diagnosed on the basis of elevated blood sugar alone, this is only the tip of the iceberg. Until recently, inflammation has had a largely underappreciated role in the initial development of insulin resistance and the long-term progression of type 2 diabetes. There are two general categories of inflammation, acute and chronic, differentiated by intensity and duration.
Acute inflammation can best be described as the protective reaction your immune system has to infection or injury. Characterized by fever, swelling, and pain, it builds up promptly when needed and then drops back quickly when the healing is done.
Chronic Inflammation can be caused by a low grade disease like arthritis, but can also exist in people without obvious disease or symptoms. Patients with type 2 diabetes exhibit significantly higher inflammatory markers and symptoms than patients of the same weight that do not have diabetes.8 Furthermore, higher chronic levels of inflammatory markers like white blood cell count, C-reactive protein (CRP) and interleukin 6 (IL-6) are early predictors of who will develop type 2 diabetes.9
So significant chronic inflammation is not just seen in those patients that already have type 2 diabetes—it also predicts those patients who go on to develop type 2 diabetes, before their blood sugar (as measured by HbA1c) shows a diabetic elevation. Inflammation is one of the suspected causes of insulin resistance.10 Inflammation is also subsequently exacerbated by the chronically elevated blood sugar characteristic of type 2 diabetes.
Once you have type 2 diabetes, your level of inflammation is also strongly associated with the development and progression of comorbidities like heart attack and kidney disease.11 If you have type 2 diabetes, it is likely that your doctor has already measured your CRP through a simple blood test.
How is type 2 diabetes treated?
The commonly accepted treatments for type 2 diabetes are referred to as the “standard of care.” And because blood glucose monitoring is now pretty universal, reducing blood sugar (and with it eventually HbA1c) tends to be the current focus of the standard of care. But as noted above, inflammation is increasingly understood to be an important indicator of your underlying metabolic health, so a treatment that lowers both average blood glucose and biomarkers of inflammation would be preferred. Another thing to consider when evaluating your treatment options is the frequency of side effects caused by any particular method of lowering blood glucose, with special attention to severe low glucose levels (hypoglycemia). Additional things to consider include the likelihood of weight gain or loss, cost, medication use, and the treatment’s effect on fatty liver and blood lipids.
The key thing to understand about treatments for type 2 diabetes is that nearly everyone has the same ultimate goal—reducing your blood sugar. While there are many ways to reduce blood sugar, some methods are more effective than others, and they all have different side effects, risks and costs. When considering what treatment is best for you, it’s important to ask yourself a few questions.
What degree of cost, risk, and side effects are you willing to take on? And can you stick with this treatment long-term?
It’s also important to recognize that not all diabetes treatments work the same—some methods only treat the symptoms of diabetes (high blood sugar), while others treat the root causes, insulin resistance and inflammation.
How does the standard of care treatment progress over the course of your life?
In early stages, many patients are recommended to start with lifestyle changes like exercising more and eating less. As the disease progresses, patients typically start taking medications. The first line of pharmaceutical therapy focuses on indirectly reducing blood sugar through pathways other than increasing insulin. If that fails, the second line of therapy is medications that increase insulin to reduce blood sugar (sulfonylureas like glipizide, and insulin). The next stage is to inject exogenous insulin (not made by your own body) using shots, a pump, or even a nasal inhaler.
Diabetes reversal vs. diabetes management
Reversal
This approach is not yet mainstream as not all medical professionals believe that diabetes can be reversed. Regardless of what the consensus is, there are peer-reviewed, published studies demonstrating diabetes reversal. Although not in lifetime cohorts (the longest prospective study is for 1 year), there are many case reports of people with prior type 2 diabetes maintaining normal blood glucose levels off medications for years or decades. These don’t claim to be cures for a reason—for most of these patients, if they stray from the regular application of the treatment and return to their previous behavior, their diabetes typically comes back.
Since there is no cure for type 2 diabetes, when evaluating your treatment options, the most important question to ask yourself is: can I stick with this intervention for the rest of my life?
Management
Management strategies focus on treating symptoms by indirectly reducing blood sugar in the short term.
Remember that blood sugar is a symptom of the underlying problem of insulin resistance and carbohydrate intolerance, so when you manage diabetes by indirectly reducing blood sugar, you are only treating the symptoms of your disease. While reducing blood sugar can protect you from the negatives effects of chronic high blood sugar, you have to stay on top of your management strategies for them to be effective—or else your blood sugar will remain high.
Type 2 diabetes treatments
There are many treatment options for type 2 diabetes. Some focus on management and some focus on reversal, and they vary in terms of efficacy, long-term sustainability, risks and monetary costs.
Reversal Strategies
Diet
Surgery
Management Strategies
Exercise
Diet
Medications that do not increase insulin
Medications that increase insulin
Low = $0 - $100 per month, Moderate = $100 - $500 per month, High = $500+ per month
*Drug prices depend on insurance coverage
For the latest on Virta's clinical trial and type 2 diabetes research efforts, visit our research page.
- Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and Trends in Diabetes Among Adults in the United States, 1988-2012. JAMA. 2015;314(10):1021-1029.
- Centers for Disease Control and Prevention. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States, 2014. Atlanta, GA: US Department of Health and Human Services; 2014.
- Tabák AG, Herder C, Rathmann W, Brunner EJ, Kivimäki M. Prediabetes: A high-risk state for developing diabetes. Lancet. 2012;379(9833):2279-2290. doi:10.1016/S0140-6736(12)60283-9.
- CDC, 1/2017
- Szabat M, Lynn FC, Hoffman BG, Kieffer TJ, Allan DW, James D. Johnson JD. Maintenance of β-Cell Maturity and Plasticity in the Adult Pancreas. Diabetes 2012; 61:1365-1371. https://doi.org/10.2337/db11-1361
- Eddy D, Schlessinger L, Kahn R et al. Relationship of insulin resistance and related metabolic variables to coronary artery disease: a mathematical analysis. Diabetes Care 2009;32(2):361–6. doi: 10.2337/dc08-0854
- Kristina M. Utzschneider, Steven E. Kahn; The Role of Insulin Resistance in Nonalcoholic Fatty Liver Disease, The Journal of Clinical Endocrinology & Metabolism, Volume 91, Issue 12, 1 December 2006, Pages 4753–4761, https://doi.org/10.1210/jc.2006-0587
- Karin E. Bornfeldt and Ira Tabas. Insulin Resistance, Hyperglycemia, and Atherosclerosis. Cell Metab; 14: 575–585. doi: 10.1016/j.cmet.2011.07.015
- Evanthia Diamanti-Kandarakis Andrea Dunaif. Insulin Resistance and the Polycystic Ovary Syndrome Revisited: An Update on Mechanisms and Implications. Endocrine Reviews. 2012; 33:981–1030. https://doi.org/10.1210/er.2011-1034
- Alan R. Saltiel and Jerrold M. Olefsky. Inflammatory mechanisms linking obesity and metabolic disease. J CLin Invest 2017; 127:1-5.
- Pradhan AD, Manson JE, Rifai N, Buring JE, Ridker PM. C-Reactive Protein, Interleukin 6, and Risk of Developing Type 2 Diabetes Mellitus. JAMA. 2001;286(3):327–334. doi:10.1001/jama.286.3.327
- Shoelson, S. E., Lee, J. & Goldfine, A. B. Inflammation and insulin resistance. J. Clin. Invest. 116, 1793–1801 (2006).
- Esser N, Legrand-Poelsa S, Piettea J, Scheen AJ, Paquot N. Inflammation as a link between obesity, metabolic syndrome and type 2 diabetes.. Diabetes Research and Clinical Practice , Volume 105 , Issue 2 , 141–150
- McKenzie AL, Hallberg SJ, Creighton BC, Volk BM, Link TM, Abner MK, Glon RM, McCarter JP, Volek JS, Phinney SD. A Novel Intervention Including Individualized Nutritional Recommendations Reduces Hemoglobin A1c Level, Medication Use, and Weight in Type 2 Diabetes. JMIR Diabetes 2017;2(1):e5. DOI: 10.2196/diabetes.6981
- Snorgaard O, Poulsen GM, Andersen HK, et al. Systematic review and meta-analysis of dietary carbohydrate restriction in patients with type 2 diabetes. BMJ Open Diabetes Research and Care 2017;5:e000354. doi: 10.1136/bmjdrc-2016-000354.
- Kodama S, Saito K, Tanaka S, et al. (2009). Influence of Fat and Carbohydrate Proportions on the Metabolic Profile in Patients With Type 2 Diabetes: A Meta-Analysis. Diabetes Care, 32(5), 959-965. doi:10.2337/dc08-1716.
- Bueno N, De Melo I, De Oliveira S, & Da Rocha Ataide T. (2013). Very-low-carbohydrate ketogenic diet v. low-fat diet for long-term weight loss: A meta-analysis of randomised controlled trials. British Journal of Nutrition, 110(7), 1178-1187. doi:10.1017/S000711451300054.
- Ajala O, English P, Pinkney J, et al. (2013). Systematic Review and Meta-Analysis of Different Dietary Approaches to the Management of Type 2 Diabetes. American Journal of Clinical Nutrition, 97(3), 505–516. doi:10.3945/ajcn.112.042457.
- Feinman R, Pogozelski WK, Astrup A, et al. (2015). Dietary Carbohydrate Restriction as the First Approach in Diabetes Management: Critical Review and Evidence Base. Nutrition, 31(1), 1–13. doi:10.1016/j.nut.2014.06.011.
- Steven S, Hollingsworth KG, Al-Mrabeh A, Avery L, Aribisala B, Caslake M, Taylor R. Very Low-Calorie Diet and 6 Months of Weight Stability in Type 2 Diabetes: Pathophysiological Changes in Responders and Nonresponders. Diabetes Care May 2016, 39 (5) 808-815; DOI: 10.2337/dc15-1942
- Van Gaal, L. F., Snyders, D., De Leeuw, I. H., & Bekaert, J. L. (1985). Anthropometric and calorimetric evidence for the protein sparing effects of a new protein supplemented low calorie preparation. The American Journal of Clinical Nutrition, 41(3), 540–544.
- Marinilli Pinto, A., Gorin, A. A., Raynor, H. A., Tate, D. F., Fava, J. L., & Wing, R. R. (2008). Successful weight-loss maintenance in relation to method of weight loss. Obesity (Silver Spring, Md.), 16(11), 2456–2461. http://doi.org/10.1038/oby.2008.364
- R O Kamrath, L J Plummer, C N Sadur, M A Adler, W J Strader, R L Young, and R L Weinstein. Am J Clin Nutr July 1992 vol. 56 no. 1 255S-257S
- Hutter MM, Schirmer BD, Jones DB, et al. First report from the American College of Surgeons Bariatric Surgery Center Network: laparoscopic sleeve gastrectomy has morbidity and effectiveness positioned between the band and the bypass. Ann Surg 2011; 254:410.
- Sjöström L et al. Association of Bariatric Surgery With Long-term Remissionof Type 2 Diabetes and With Microvascularand Macrovascular Complications. JAMA. 2014;311(22):2297-2304
- Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA 2004; 292:1724.
- Brito JP, Montori VM, Davis AM. Metabolic Surgery in the treatment algorithm for type 2 diabetes: a joint statement by international diabetes organizations. JAMA. 2017; 317(6):635-636
- Chang SH, Stoll CR, Song J, et al.The effectiveness and risks of bariatric surgery.JAMA Surg. 2014;149(3):275-287.
- Rubino F, Nathan DM, Eckel RH, et al. Metabolicsurgery in the treatment algorithm for type 2 diabetes.Diabetes Care. 2016;39(6):861-877.
- Hashimoto Y, Fukuda T, Oyabu C, Tanaka M, Asano M, Yamazaki M, Fukui M. Impact of Low-Carbohydrate Diet on Body Composition: Meta-Analysis of Randomized Controlled Studies. Obes Rev. 2016;17(6):499-509
- Tobias DK, Chen M, Manson JE, Ludwig DS, Willett W, Hu FB. Effect of Low-Fat Diet Interventions Versus Other Diet Interventions on Long-Term Weight Change in Adults: A Systematic Review and Meta-Analysis. Lancet Diabetes Endocrinol. 2015 ;3(12):968-79



