New Recommendations for HbA1C Targets for Type 2 Diabetes: Warranted or Short-Sighted?

Hemoglobin A1c (HbA1c) has been a standard test of long-term average blood glucose control for patients with type 2 diabetes (T2D) for more than a decade, and blood levels above accepted thresholds are used to diagnose both pre-diabetes (between 5.7 and 6.4%) and diabetes (above 6.4%). While it is uniformly accepted that higher HbA1c levels are associated with greater risk of complications from diabetes, as well as the incidence of other diseases, the targets for reducing this biomarker in people with existing diabetes remain open to debate. In particular, aggressive pharmaceutical therapy increases both side effects and costs, which need to be considered when assessing the net benefits accrued from meeting specific HbA1c targets.
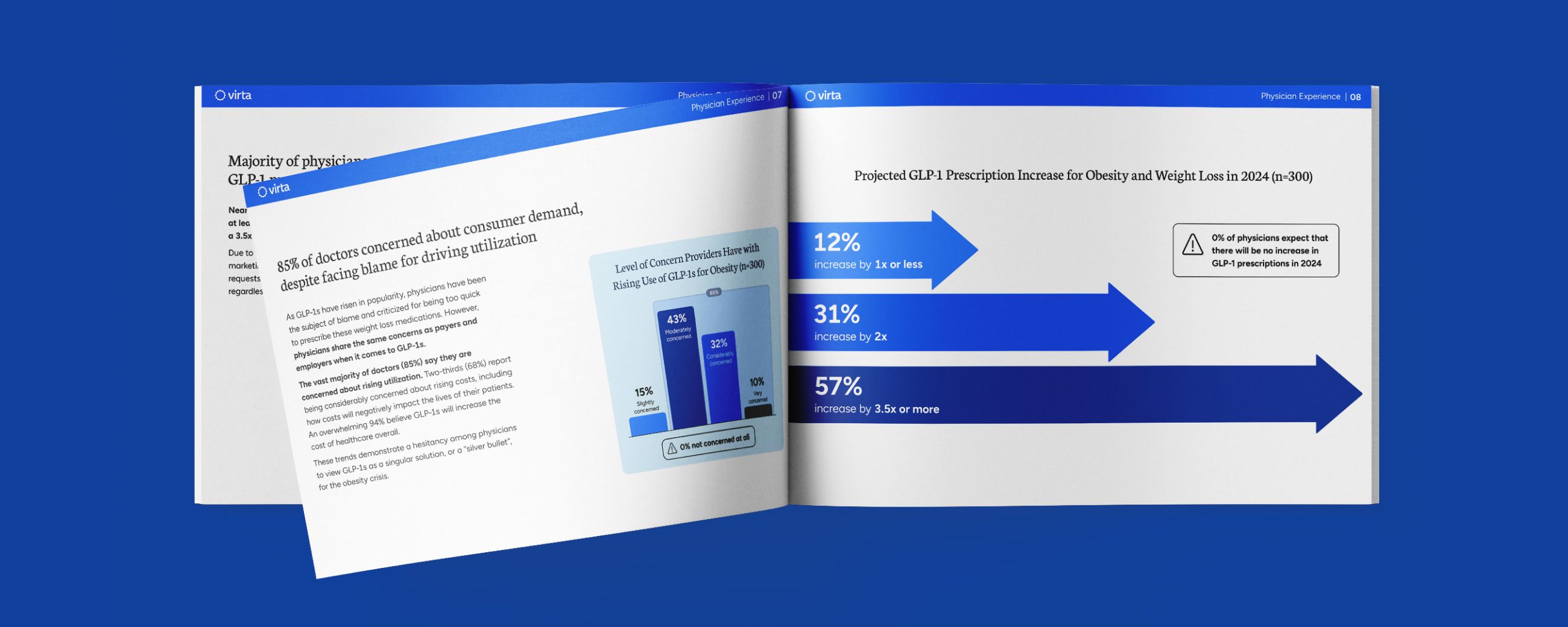
Recently the American College of Physicians (ACP) published less stringent treatment goals than those advocated by the American Diabetes Association (ADA), resulting in an open debate between these two trusted medical organizations. As you might expect, this is of considerable interest to us at Virta as we strive to help our patients achieve even lower HbA1c values than either of these organizations recommend.
So are we going to change our treatment goals? This is a complex consideration, but the simple answer is no. Whereas the current standard of care for T2D relies upon increased medications to reach HbA1c goals, Virta leverages the beneficial biochemistry of nutritional ketosis to improve metabolic health. And in the process of achieving major HbA1c reductions, we also reduce or stop a majority of the medications for most individuals, resulting in reduced medication side effects and costs.
In other words, the method used to get to a specific HbA1c level will significantly affect the resulting risk-benefit ratio, and thus the appropriate targets will differ depending on the chosen method of treatment. So here, in detail, is how we at Virta justify setting an HbA1c target reflecting better blood glucose control than what is advocated by either the ACP or the ADA.
Perspective on Treatment Targets
Medical treatment guidelines reflect an extensive body of research and the time-tested input from leading experts within a given field. The expectation we all have is that this process provides recommendations that are reflective of best practice for the general patient population they address. Ideally, these guidelines provide a framework for treatment, and then they are individualized to best meet the needs of the patient and their unique physiology and lifestyle. The approach to handling T2D is no different. In addition to medical intervention, how we eat, move, sleep and think all have the power to dramatically influence our health. What we know and how we approach the treatment of T2D is a dynamic and evolving process, but a thorough understanding of the treatment targets for the disease and how they influence the possible outcomes for patients must be our ultimate guide on the journey to wellness.
HbA1c: A Peek Under the Hood
Wellness incorporates many aspects of health and well-being and means something different to everyone. One way in which we quantify metabolic wellness is by measuring HbA1c values.
This measure of glycosylated hemoglobin has been used as one of the key biomarkers in identifying patients with T2D for more than a decade. HbA1c serves as a reflective measure of blood glucose values over a period of about 12 weeks, and when elevated above 6.4%, is indicative of severely impaired glycemic control. This value helps us recognize when the tools the body has to utilize and store glucose aren’t working properly.
Important Definitions:
Microvascular damage affects your small blood vessels—like those in yours eyes and kidneys. Complications include loss of vision, impaired kidney function and amputations
Macrovascular damage affects large blood vessels—like those in your heart and brain. Complications include heart attacks and strokes.
Therefore, a repeated HbA1c value of 6.5% or greater is an established diagnostic and treatment metric for patients with diabetes. The significance of this number comes into play when we see how persistent elevations in blood glucose can lead to damaged blood vessels.
Navigating the Targets for HbA1c
With more than 100 million U.S. adults living with diabetes and prediabetes,¹ the value of education and treatment for this condition cannot be overstated. The health and economic costs of managing, rather than improving, the complications associated with diabetes necessitate a careful look at the treatment options that are available for this disease.
Over the past ten years the American Diabetes Association (ADA) recommendations for glycemic control have consistently targeted HbA1c values of less than 7%,² pointing to the vascular benefits of maintaining HbA1c in this range while remaining mindful of the risks of hypoglycemia. The American Association of Clinical Endocrinologists and American College of Endocrinology (AACE/ACE) and the Department of Veterans Affairs (VA/DOD) have also recommended values of less than 7% in patients without contraindications, comorbid conditions and / or limited life expectancy.³,⁴ In March of 2018, however, the American College of Physicians (ACP) recommended a notable shift from this treatment target with the release of their Guidance Statement entitled Hemoglobin A1c Targets for Glycemic Control with Pharmacologic Therapy For Nonpregnant Adults with Type 2 Diabetes Mellitus.⁵ This guidance recommends clinicians loosen the tight control parameters established for HbA1c from a target of less than 7% to a range between 7–8%. The statements were based on their review of the scientific literature combined with a review of other organizations’ guidelines pertaining to HbA1c targets in non-pregnant adults with T2D.
Summary of Recommendations from the ACP Guidance Statement:⁵
- Clinicians should personalize goals for glycemic control
- Aim to achieve HbA1c 7–8% in most patients
- De-intensify pharmacologic therapy when HbA1c < 6.5%
- Avoid targeting HbA1c level in certain patient populations
The ACP determined that the risks associated with intensive medication therapy aimed at achieving tight HbA1c control were greater than the benefits, asserting that the evidence did not support enough of an improvement in outcomes for patients with an HbA1c of less than 7% versus 7–8%. The statement cited concerns with intensive pharmacologic treatment as it relates to adverse events, medication costs and patient burden, as well as the risk-benefit analysis based upon a patient’s health status.⁵ According to the ACP, their guidance statement is consistent with the recommendations of the Institute for Clinical Systems Improvement (ICSI) guideline from 2014 wherein a recommendation for >7% – <8% was provided in order to manage the potential complications of intensive medication therapy.⁶
In their Guidance Statement 2, the ACP does acknowledge, however, that these recommendations are based on the effects of pharmacologic treatment and that lower targets for glycemic control may be appropriate if achieved via dietary changes and lifestyle modifications like exercise and weight loss. While this guidance goes against years of substantial evidence-based recommendations, the identification of the potential efficacy of diet and exercise intervention may be one positive, albeit small, take-away from this controversial update.
In light of the abrupt shift in the long-standing, and well-supported advice to target HbA1c levels below 7%, the ADA promptly issued a statement expressing “deep concern” over the ACP’s 2018 Guidance Statement. The ADA reiterated the importance of individualization in any treatment decision for patients with T2D and the avoidance of blanket recommendations based on risks for susceptible members of the patient population. The rebuttal points to the established body of evidence that supports a reduction in HbA1c below 7% to mitigate diabetes-related complications and cardiovascular disease outcomes. The ADA further states that de-intensification or simplification of medication regimens for older adults may be appropriate; however, no lower limit HbA1c value for de-intensification has been established for general patients if appropriate measures are taken to minimize the risks of hypoglycemia.⁷
All of the existing guidelines the ACP used to develop their guidance statements recommend an HbA1c value less than 7% in the absence of serious medical circumstances or very advanced age. One of the most important factors to highlight is that these recommendations are based primarily on the potential deleterious side-effects of intensive pharmacologic treatment. That is to say, taking a lot of medications to manage T2D can be risky, and may do more harm than you would think. Diet and lifestyle modifications are also mentioned and recommended throughout the various referenced guidelines, but no direction is given as to what this means or how to implement them. We recognize that this may be due in part to the newness of the published results from the Virta Treatment, such that these expert panels have yet to appreciate how truly powerful nutritional ketosis can be in treating the underlying cause of T2D (i.e., inflammation and insulin resistance), while simultaneously reducing medication use with its associated costs and side effects.
Your Health Now and in the Future
Now, you may be asking, does a target range of 7–8% rather than less than 7% really make a difference? It sounds like we are splitting hairs here. Unfortunately, the numbers do matter. Even if slight, a chronic elevation of HbA1c has been implicated in many diseases due in part to the signals that high blood glucose send out to the body. So, while the risk of hypoglycemic events is a serious concern that can accompany medication therapy for T2D, chronic hyperglycemia is also an issue with serious health implications.
We mentioned the common complications of poorly controlled T2D that include retinopathy, nephropathy, and neuropathy, plus heart attack and stroke—no doubt a scary list! However, compelling research has also implicated hyperglycemia, as reflected in elevated HbA1c, as an independent epigenetic trigger⁸ as well as a predictor of certain cancers.⁹
You may have heard the term ‘epigenetics’ lately, but what exactly does it mean and what role does it play in T2D? Epigenetics is the complex interaction between genes and the environment. In other words, environmental influences (like diet) and heritable factors (like the potential for elevated HbA1c) can impact the expression of our genes as it relates to health and disease.⁸,¹⁰,¹¹
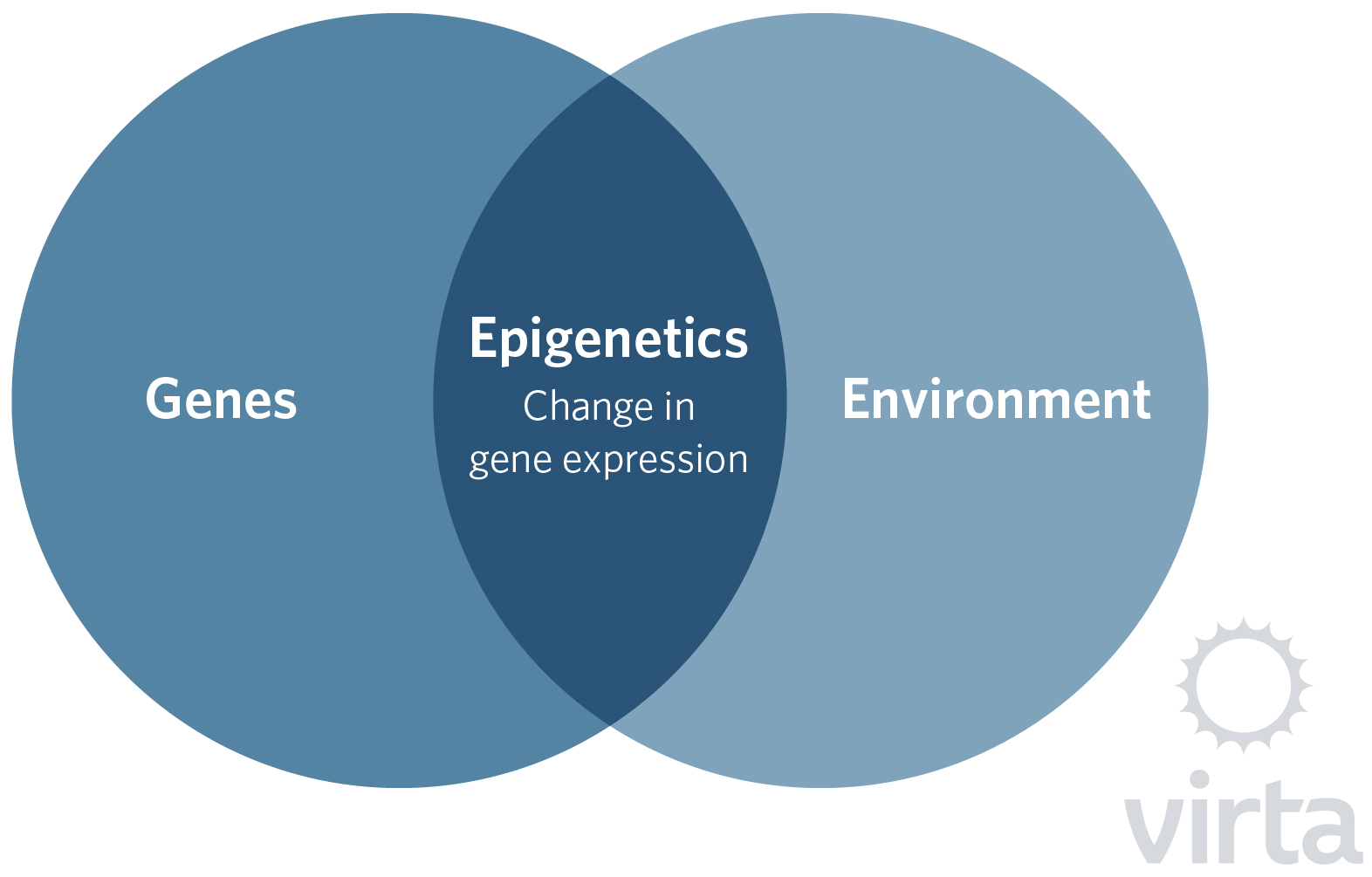
Hyperglycemia is one of many environmental factors that can lead to epigenetic modifications. One of the more well-known modifications is DNA methylation. Bear with us on the science here, but it is important in understanding why epigenetics matters when making decisions about treating T2D. DNA methylation is a process by which a methyl group is added to a molecule, and in doing so can alter gene functions, most often by reducing gene expression. This reduction doesn’t always mean a reduction in bodily processes; for example, it can also result in the increase of a particular process. For instance, turning off an anti-inflammatory gene may promote inflammation.
This takes us back to the signals that hyperglycemia can send out to the body. In humans, DNA methylation is influenced by diet and exercise and therefore it has been speculated that it may be involved in lifestyle-related diseases.¹¹ Though DNA methylation is a normal process through which the body regulates its day-to-day functions, a persistent alteration in DNA methylation can result in metabolic perturbations that further contribute to diabetes-related complications.⁸
For example, researchers have identified an association between elevated levels of HbA1c and an increase in DNA methylation that specifically reduces insulin production by the beta cells of the pancreas.⁸,¹² This sets up what is essentially a biochemical vicious cycle. We have elevated blood glucose that leads to increased HbA1c which then tells the pancreas to make less of the insulin needed to move glucose into the cells.
If that weren’t enough to question whether or not it is a good idea to maintain a higher HbA1c target, elevated HbA1c may also independently predict increased risk of certain cancers, like colorectal, gastric, pancreatic, liver and possibly breast cancers as well as increase the risk of a higher cancer stage.⁹ A meta-analysis of many different studies, examining the relationship between cancer and measures of HbA1c found a positive linear correlation between increased HbA1c values and the incidence of the above-mentioned cancers.⁹ This means that as HbA1c goes up, so does the risk of these cancers. Insulin,¹³ inflammation,¹⁴ the affinity of certain cancers cells for glucose¹⁵,¹⁶ and the activation of oncogenic (tumor-causing) pathways resulting from hyperglycemia.¹⁷ These are all possible mechanisms connecting HbA1c and cancer. Thus, the evidence continues to mount for the benefits of achieving and maintaining glycemic control with HbA1c values under 6.5–7% to mitigate these risks.
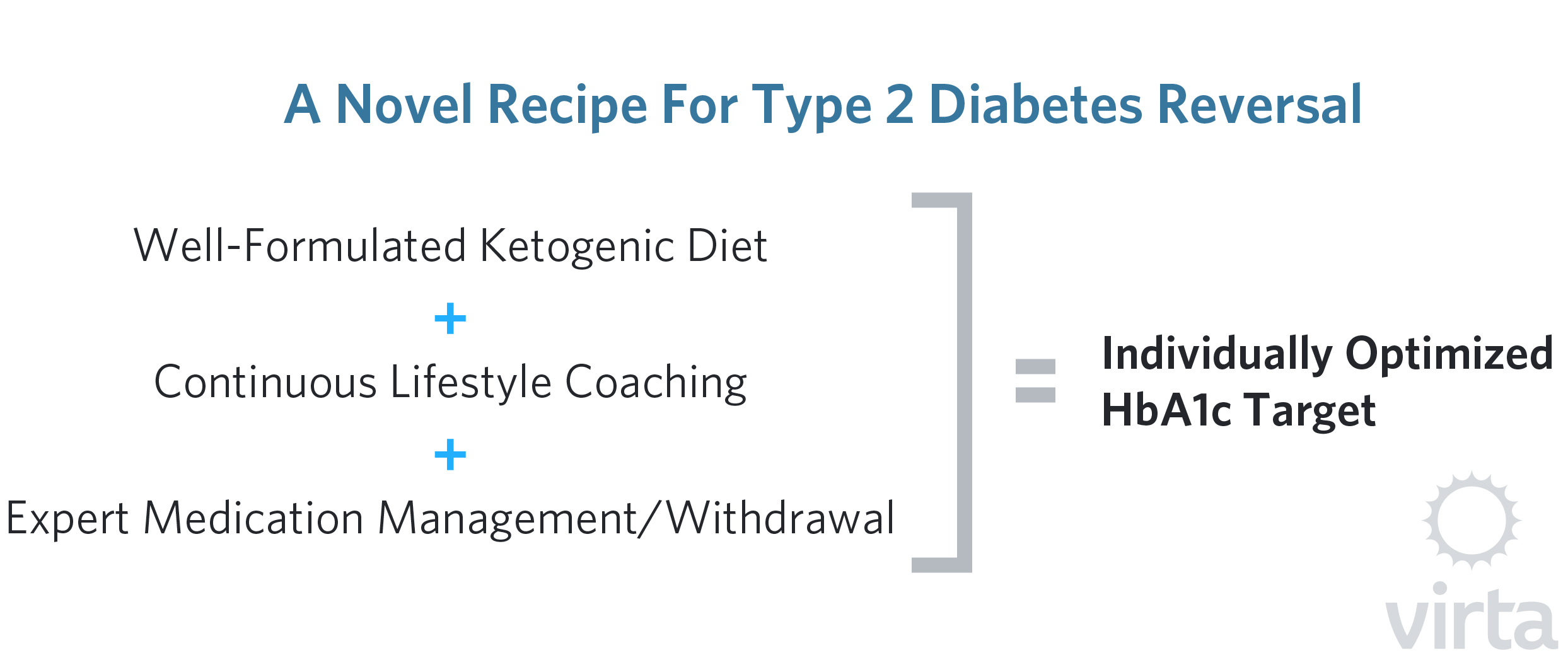
A Novel Recipe For Type 2 Diabetes Reversal
What we have presented so far is the difficult balancing act between the risks of letting HbA1c remain above 7% and the risks of pushing it down below 7% with intensive medication use. But clearly this picture is not all doom and gloom! Unlike the traditional low fat diets that do not have any lasting effect on T2D, the Virta Treatment using a well-formulated ketogenic diet, can trigger a ‘virtuous cycle’ by its own epigenetic effects that turn on and off our genes in the direction of good health and longevity.¹⁸
A continually growing body of scientific literature supports the use of a low carbohydrate and/or a well-formulated ketogenic diet approach to treating T2D and improving glycemic control. As more longitudinal studies are performed, additional information has been made available concerning the sustained benefits of treatment approaches that incorporate dietary and behavioral strategies to facilitate compliance and integrity of the diet to achieve the desired results.¹⁹,²⁰,²¹
Our recent publication of the one-year results of the Virta Treatment utilizing a well-formulated ketogenic diet showed an average reduction in HbA1c values from 7.6% to 6.3%. Many of these reductions were achieved within 70 days of the onset of treatment and some of the patients were able to completely eliminate or significantly reduce their medications.¹⁸ These interventions have the dual benefit of reducing hyperglycemia while also mitigating the serious concern of medication-induced hypoglycemic events, not to mention reduced prescription costs and the patient burden associated with frequent medication dosing.
Summary
Elevated HbA1c is an important indicator of chronically elevated blood glucose and it participates in a cascade of health consequences from vascular damage and the resultant pathologies, as well as increased risk of certain cancers. Long-standing recommendations from the ADA as well as AACE/ACE and the VA/DOD have established a target range of below 7% for most patients not presenting with contraindications to treatment. New recommendations by the ACP to increase that range may be short-sighted when taking into account the multifactorial short and long range ramifications of our body’s tissues being subjected to chronic hyperglycemic conditions.
Although tight control of blood glucose levels achieved through intensive medication use may warrant careful scrutiny on an individual basis and pose an increased risk to some patients, we need to recognize that current pharmaceuticals and the biochemistry of nutritional ketosis work via fundamentally different pathways. It is also true that to be safe and effective, a well-formulated ketogenic diet requires expert health coaching with careful medication management, but we have now demonstrated its potential to effect dramatic health improvements and a reduction in the risks of a myriad of associated complications. This unique ability of the Virta Treatment to reduce HbA1c while reducing insulin resistance, inflammation, body weight, and the risk of symptomatic hypoglycemia puts our treatment into a completely different class that is clearly in need of its own HbA1c goals.
As thousands of T2D patients go through the Virta Treatment, we will further sharpen our ability to guide each individual to their best, sustainable HbA1c target. But for now our Indiana University Health Study results demonstrate that after a year, a majority of our patients are sustaining HbA1c values less than 6.5% off their diabetes medications and with dramatically improved metabolic health. These few hundred pioneers are proving that there can be life and health after diabetes.
The information we provide at virtahealth.com and blog.virtahealth.com is not medical advice, nor is it intended to replace a consultation with a medical professional. Please inform your physician of any changes you make to your diet or lifestyle and discuss these changes with them. If you have questions or concerns about any medical conditions you may have, please contact your physician.
This blog is intended for informational purposes only and is not meant to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition or any advice relating to your health. View full disclaimer
Are you living with type 2 diabetes, prediabetes, or unwanted weight?

- Centers for Disease Control and Prevention. New CDC report: More than 100 million Americans have diabetes or prediabetes. https://www.cdc.gov/media/releases/2017/p0718-diabetes-report.html. Published July 18, 2017.
- American Diabetes Association. Standards of medical care in diabetes – 2018. Diabetes Care. 2018;41(Suppl. 1):S1-S159.
- AACE/ACE Diabetes Guidelines, Endocr Pract. 2015;21(Suppl 1):1-87.
- Department of Veterans Affairs and Department of Defense. VA/DoD Clinical Practice Guideline for the Management of Type 2 Diabetes Mellitus in Primary Care. https://www.healthquality.va.gov/guidelines/CD/diabetes/VADoDDMCPGFinal508.pdf. Published April 2017. Accessed March 25, 2018.
- Qaseem A, Wilt TJ, Kansagara D, et al. Hemoglobin A1c targets for glycemic control with pharmacologic therapy for nonpregnant adults with type 2 diabetes mellitus: a guidance statement update from the American College of Physicians. [published online ahead of print March 06, 2018]. Ann Intern Med. doi: 10.7326/M17-0939.
- Redmon B, Caccamo D, Flavin P, Michels R, O’Connor P, Roberts J, et al; Institute for Clinical Systems Improvement. Diagnosis and Management of Type 2 Diabetes Mellitus in Adults. 16th ed. Bloomington, MN: Institute for Clinical Systems Improvement; July 2014.
- American Diabetes Association® deeply concerned about new guidance from American College of Physicians regarding blood glucose targets for people with type 2 diabetes. American Diabetes Association. http://www.diabetes.org/newsroom/press-releases/2018/ada-acp-guidance-response.html. Published March 08, 2018. Accessed March 25, 2018.
- Yang BT, Dayeh TA, Kirkpatrick CL, et al. Insulin promoter DNA methylation correlates negatively with insulin gene expression and positively with HBA1c levels in human pancreatic islets. Diabetologia. 2011;54(2):360-367.
- de Beer JC, Lienbenberg L. Does cancer risk increase with HbA1c, independent of diabetes? Br J Cancer. 2014;110(9):2361-2368.
- Rönn T, Volkov P, Gillberg L, et al. Impact of age, BMI and HbA1c levels on the genome-wide DNA methylation and mRNA expression patterns in human adipose tissue and identification of epigenetic biomarkers in blood. Hum Mol Genet. 2015;24(13):3792-3813.
- Nilsson E, Jansson PA, Perfilyev A, et al. Altered DNA methylation and differential expression of genes influencing metabolism and inflammation in adipose tissue from subjects with type 2 diabetes. Diabetes. 2014;63(9):2962-2976.
- German MS, Moss LG, Rutter WJ. Regulation of insulin gene expression by glucose and calcium in transfected primary islet cultures. J Biol Chem. 1990;265(36):22063-22066.
- Saydah SH, Platz EA, Rifai N, Pollak MN, Brancati FL, Helzlsouer KJ. Association of markers of insulin and glucose control with subsequent colorectal cancer risk. Cancer Epidemiol Biomarkers Prev. 2003;12(5): 412–418.
- Habib SL, Rojna M. Diabetes and risk of cancer. ISRN Oncol 2013: 583786.
- Hanahan D, Weinberg. Hallmarks of cancer: the next generation. Cell 2011;144(5): 646–674.
- Mathews EH, Liebenberg L. Short-term starvation for cancer control in humans. Exp Gerontol 2013;48(11): 1293.
- Onodera Y, Nam JM, Bissell MJ. Increased sugar uptake promotes oncogenesis via EPAC/RAP1 and O-GlcNAc pathways. J Clin Invest. 2014;124(1): 367–384.
- Newman JC, Verdin E. β-hydroxybutyrate: Much more than a metabolite. Diabetes Res Clin Pract. 2014; 106(2):173-181.
- Hallberg SJ, McKenzie AL, Williams PT, et al. Effectiveness and safety of a novel care model for the management of type 2 diabetes at 1 year: an open-label, non-randomized, controlled study [published online ahead of print February 07, 2018]. Diabetes Ther. doi: 10.1007/s13300-018-0373-9.
- Saslow LR, Daubenmier JJ, Moskowitz JT, et al. Twelve-month outcomes of a randomized trial of a moderate-carbohydrate versus very low-carbohydrate diet in overweight adults with type 2 diabetes mellitus or prediabetes. Nutr Diabetes. 2017;7(12):304.
- Saslow LR, Mason AE, Kim S, et al. An online intervention comparing a very low-carbohydrate ketogenic diet and lifestyle recommendations versus a plate method diet in overweight individuals with type 2 diabetes: a randomized controlled trial. J Med Internet Res. 2017;19(2):e36.