Improving sleep through carbohydrate restriction and nutritional ketosis

Sleep disturbances and their effect on health, economic burden, and glucose control
Sleep deprivation and sleep disorders decrease the effectiveness of your immune system, making you more likely to get sick. Sleep deprivation affects mood, focus, and decision-making, decreasing productivity and making people more likely to get into accidents. It also impacts metabolic health by decreasing insulin sensitivity (1). Sleep deprivation is a global issue, with an estimated $411 billion lost or 2.28% of the GDP per year in the US alone (2).
The Virta Treatment improved sleep quality
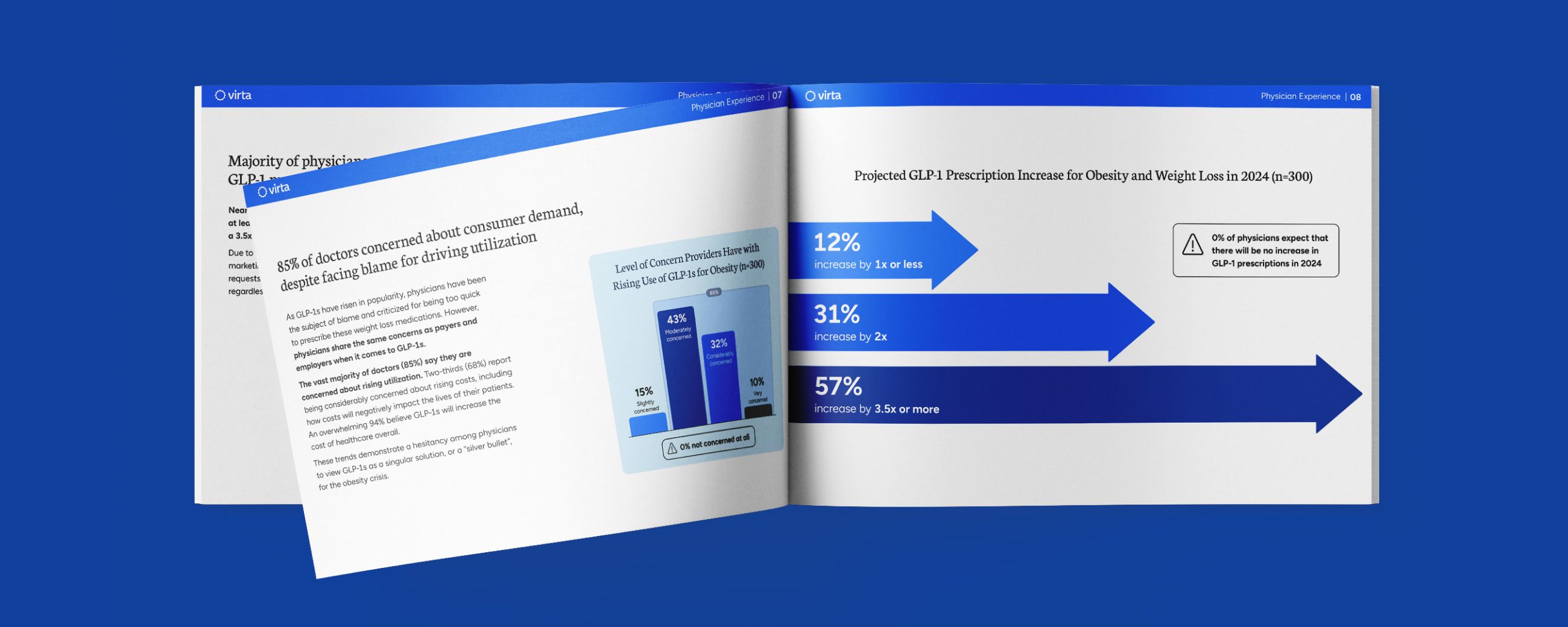
In the Indiana University Health Diabetes Clinical Trial, patients receiving the continuous care intervention arm of the Virta Treatment showed significant improvements in sleep (3). Sleep quality was measured using a standard sleep questionnaire called the Pittsburgh Sleep Quality Index (PSQI). The PSQI accesses 7 components of sleep quality.
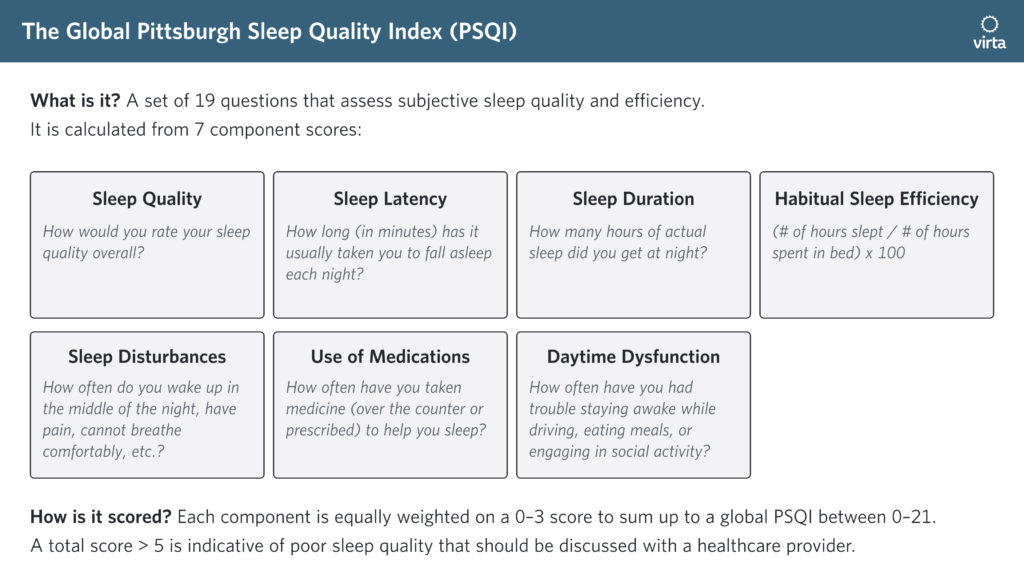
The Virta treatment improved overall global PSQI as well as subjective sleep quality (component 1), sleep disturbance (component 5), and daytime dysfunction (component 7). The chart below shows the percent change between baseline and 1 year in sleep measures.

These results show that the Virta Treatment was not only effective in improving glycemic control, weight, cardiovascular outcomes, and liver outcomes, it also improved overall sleep quality and daytime functioning in patients with type 2 diabetes (T2D). Both the American Diabetes Association (ADA) and International Diabetes Federation (IDF) recommend a sleep assessment as part of the annual evaluation for patients with type 2 diabetes and encourages treatment for those with obstructive sleep apnea or any other sleep disorders (4,5). Here, while reversing diabetes and improving glycemic control, we demonstrated an additional benefit of overall sleep quality improvement in patients receiving the Virta Treatment with the continuous care intervention.
Why is sleep improvement important for type 2 diabetes management?
It is estimated that more than half of T2D patients have some kind of sleep disturbance, while one-third of them have sleep-disordered breathing (SDB) (4). SDB, especially obstructive sleep apnea (OSA), is frequently found in patients with type 2 diabetes (5,6). Obesity is a common risk factor in both SDB and T2D. Obesity likely contributes to the pathogenesis of both conditions (7). However, there is some evidence that these two conditions may be directly related to each other, independent of obesity (8). The interrelationship between T2D and SDB not only affects the overall quality of life, but also presents with other clinical consequences by increasing the likelihood of these patients developing hypertension and cardiovascular complications (9,10).
Lifestyle intervention resulting in weight loss is recommended for all OSA patients, regardless of whether the patients are receiving other treatments to improve sleep (5,6). The Virta Treatment reported an average 12% weight loss at one year and showed a positive impact in sleep quality as well. Not only did it improve diabetes symptoms in both T2D and prediabetes patients, it also resolved poor sleep in 11.8% and 29.2% of patients with T2D and prediabetes. This additional benefit observed by the Virta Treatment patients may be related to the degree of weight loss experienced by these patients. In a previous study, it has been shown that a weight loss of 10kg or more had the most benefit with OSA improvements (11).
An intervention that improves several branches of metabolic alterations
It is evident that the Virta Treatment, using carbohydrate restriction with nutritional ketosis and weight loss, improved overall sleep quality in patients with T2D and prediabetes. The ability to improve sleep while improving glycemic control, cardiovascular disease and non-alcoholic fatty liver disease risk in the Virta Treatment shows the effectiveness of this intervention to act simultaneously in several branches of metabolic alterations. This comprehensive effect by the Virta Treatment is an attractive alternative for patients with T2D to consider for treating their diabetes status and other underlying conditions such as sleep disruption. The present study assessed sleep using self-reported subjective sleep measures. Future studies evaluating sleep using polysomography or portable devices such as actigraphy are needed to confirm and expand on the benefit of the Virta Treatment in treating sleep disturbances.
The information we provide at virtahealth.com and blog.virtahealth.com is not medical advice, nor is it intended to replace a consultation with a medical professional. Please inform your physician of any changes you make to your diet or lifestyle and discuss these changes with them. If you have questions or concerns about any medical conditions you may have, please contact your physician.
This blog is intended for informational purposes only and is not meant to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition or any advice relating to your health. View full disclaimer
Are you living with type 2 diabetes, prediabetes, or unwanted weight?

- Spiegel KS, Leproult R and Van Cauter E. Impact of a sleep debt on metabolic and endocrine function. The Lancet 1999; 354: 1435-1439
- Hafner M, Stepanek M, Taylor J, et al. Why sleep matters-the economic costs of insufficient sleep: A cross-country comparative analysis. RAND Europe 2016. www.rand.org/t/RR1791.
- Siegmann M, Athinarayanan S, Hallberg S, et al. Improvement in patient-reported sleep in type 2 diabetes and prediabetes participants receiving a continuous care intervention with nutritional ketosis. Sleep Medicine 2019. 55; 92-99.
- American Diabetes Association. 3. Comprehensive medical evaluation and assessment of comorbodities: Standards of medical care in diabetes. Diabetes Care 2019
- The IDF consensus statement on sleep apnoea and type 2 diabetes 2008. 1-24.
- West SD, Nicoll DJ, Stradling JR. Prevalence of obstructive sleep apnoea in men with type 2 diabetes. Thorax 2006; 61: 945-950.
- Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature 2006; 444: 840-846.
- Punjabi NM, Shahar E, Redline S, et al. Sleep-disordered breathing, glucose intolerance, and insulin resistance: The Sleep Heart Health Study. Am J Epidemiol 2004; 160: 521-530.
- Dineer HE, O’Neill W. Deleterious effects of sleep disordered breathing on the heart and vascular system. Respiration 2006; 73: 124-130.
- Peppard PE, Young T, Palta M, et al. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med 2000; 342: 1378-1384.
- Foster GD, Borradaile KE, Sanders MH, et al. A randomized study on the effect of weight loss on obstructive sleep apnea among obese patients with type 2 diabetes: the Sleep AHEAD study. Arch Intern Med 2009; 169: 1619-1626.