The Importance of Managing Potassium and Sodium as Part of a Well-Formulated Ketogenic Diet

Why It’s Necessary to Double Down on Sodium and Potassium
One of the biggest challenges we encounter in managing people following a ketogenic diet is to get them to pay adequate attention to their sodium and potassium intakes. Part of this stems from the past 50 years of salt demonization, in which we were all taught that the less sodium intake, the better. In our post on sodium and the myth of adrenal fatigue a year ago, we explained the fallacy of this nation-wide, low salt policy (1), particularly in the context of a well-formulated ketogenic diet.
The other barrier to gaining attention to this pair of essential minerals that doctors call ‘electrolytes’ is that potassium has been sorely neglected despite its reputation as a healthy nutrient. Since it is found in a wide range of foods, the assumption is that most people eating a ‘balanced diet’ get plenty of potassium. Moreover, no one has a patent on potassium as a supplement, so there is not a lot of profit to be made from educating and selling it to a vulnerable segment of the public who might benefit from it. And yet, there are many factors that can lead to inadequate potassium intakes (more on that below).
In brief, across the normal dietary variation for this common mineral, intakes in the lower range for the population (i.e., those in the lowest quarter) are associated with about twice the mortality risk compared to those whose potassium intakes are in the highest quarter.
When looked at from this perspective, this is rather astonishing! Here’s a common essential nutrient that could deliver remarkable health benefits for those whose daily intake is in the lower range of ‘normal.’ More importantly, when someone adopts a ketogenic diet, quite a few of the more common food sources of potassium are excluded (e.g., high sugar fruit, dried peas and beans, starchy vegetables), which tends to reduce one’s daily intake into the unhealthful range.
Thus, a well-formulated ketogenic diet (WFKD) requires a bit of attention to food choices and food preparation to maintain an optimum potassium intake. Add to this the well-characterized interactions between sodium and potassium management by the kidneys, plus the changes in sodium handling during nutritional ketosis, and this topic assumes a position of significant importance on one’s ‘to do list’ to optimize health and well-being with a WFKD.
Potassium and Mortality in the Balance
Potassium is the positively charged ion (aka electrolyte) that is predominate in the fluid inside all of the body’s cells, while sodium plays a matching role in the fluid surrounding our cells—including blood plasma. Keeping the two of them in balance is an extremely delicate and intricate process involving multiple hormones and organs, particularly the kidneys. In order for nerves and muscles to function, the concentrations of positively charged potassium (K+) and sodium (Na+) have to be essentially equal across the cell membranes. And when nerves fire or muscles contract, some of these two electrolytes are exchanged across the cell membrane, and then have to be pumped back out (Na+) or back in (K+) to prepare for more work to be done. If either this balance, or the in-and-out flow are impaired, nerves and muscles don’t work properly, endangering health and even life itself.
Because part of sodium’s role in the plasma is to maintain adequate circulation, it has been well characterized as necessary for normal blood flow. And in the case of high blood pressure, it is tempting to conclude that one just needs to restrict sodium intake to get it to come back down. While there is some truth to this (for people with salt-sensitive hypertension), for most people with high blood pressure, the story is much more complex and involves the appropriate balance between these two electrolytes rather than a focus on the intake of sodium in isolation.
There have been many attempts to study this balance, ranging from assessing the effects of short-term tightly-controlled diets, to the less rigorous technique of having large groups of people record their food intake from which intakes of Na+ and K+ are then estimated (2). Due in part to the known inaccuracies associated with self-reported food intake, conflicting or non-significant results of such studies have generated more confusion than convincing conclusions about optimum intakes for these two electrolytes.
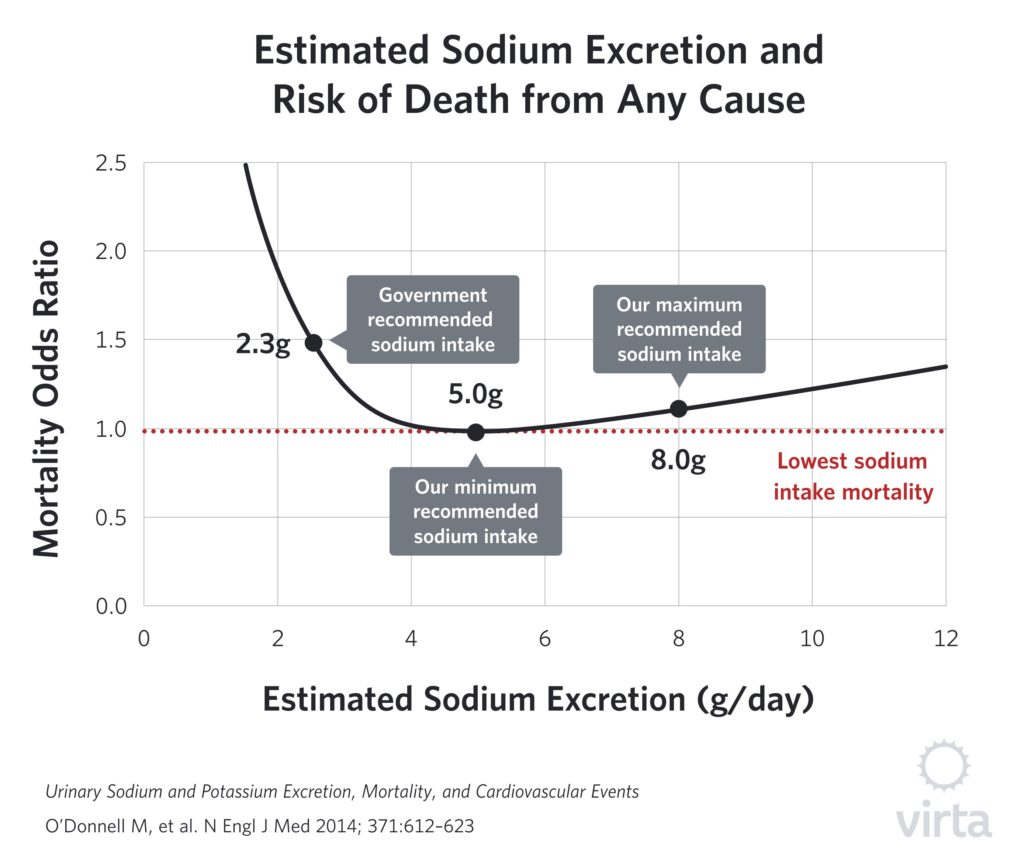
More recently, large studies have measured the actual amounts of sodium and potassium in a person’s urine as a more accurate indicator of their dietary intakes. For example, Leonberg-Yoo et al (3) observed reduced mortality with higher urinary potassium contents in patients with kidney disease. But the most definitive results to date are from the massive international PURE study reported by O’Donnell et al (4). In this study, they collected urine from 102,000 people in 17 countries and then monitored health and mortality for 4 years. As we noted in our blog post on sodium, the lowest mortality was seen in people consuming 5 grams per day, which is about twice the current US recommended guideline for healthy adults. For sodium intakes substantially above or below this value, the associated mortality rates rise, generating a U-shaped curve.
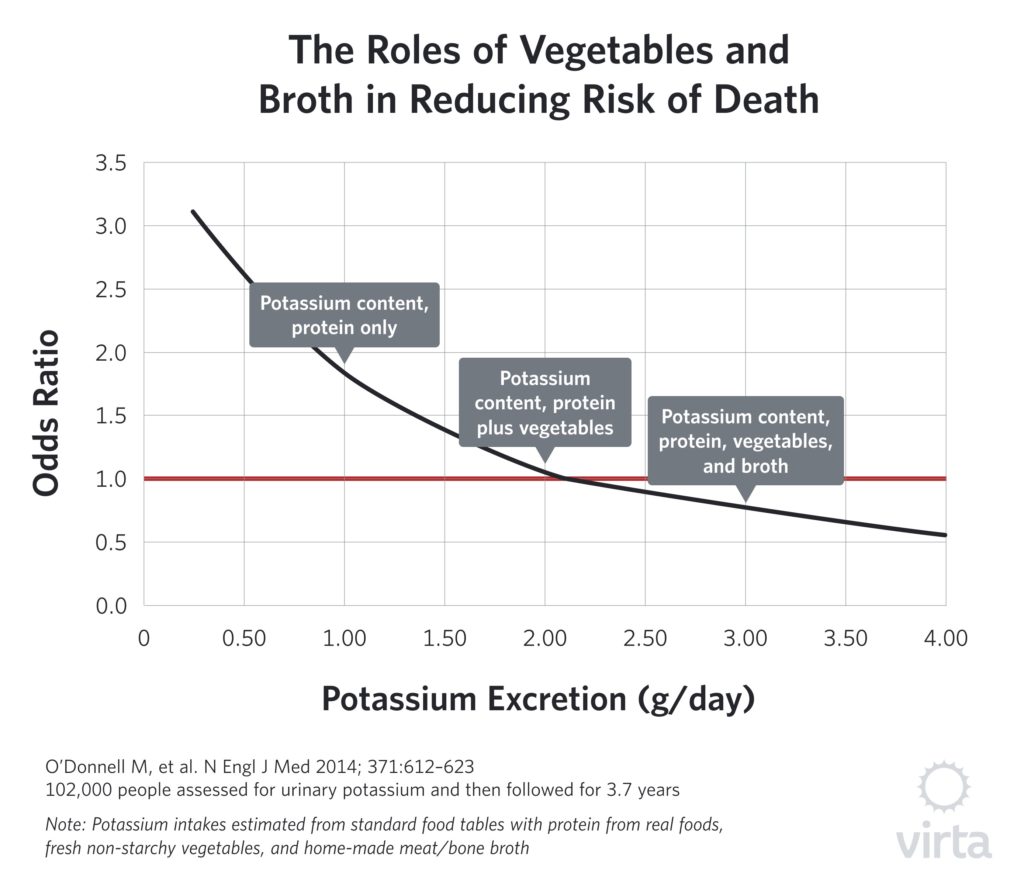
But the urinary potassium data from the PURE Study (shown here) tell a very different story. While low levels of potassium excretion are clearly associated with increased mortality risk, increasing levels in the urine up to 3-4 grams per day correlate with reduced risk. And in particular, the associated mortality at 1 gram per day is about double that seen at 3 grams per day. For this reason, we recommend incorporating real foods into a WFKD providing 3-4 grams per day of potassium.
The Relationship Between Sodium and Potassium Intakes and Urinary Excretion
Almost all of the sodium we eat gets absorbed, and then about 90% of that comes out in our urine. Therefore, urinary sodium is an accurate reflection of our dietary intake. However, this relationship between dietary intake and urinary output is not quite as good for potassium. In most people, about 75% of dietary potassium is excreted in the urine. Thus, in the studies linking urinary potassium excretion to health such as the PURE study, a correction factor of about 1.3 should be applied. This means that in order to have 2 grams of potassium come out in the urine, one would need to consume 2.6 grams in the diet, and similarly to have 3 grams in the urine would require about 4 grams of dietary intake.
Practical Health Implications of Dietary Potassium
In order to appreciate the practical significance of varying dietary potassium intakes, here are three important questions:
- Realistically, how does this compare to the amount of potassium that the average adult consumes in a day?
- Is there a meaningful percentage of the population who eat less than 3 grams per day and thus may be at increased mortality risk?
- What happens to potassium intakes when people cut out most of their typical carbohydrate-containing foods?
This table (derived from food intake data from almost 6000 US adults) shows the range in potassium intakes for the bottom 10%, the middle 50% and top 90% across the population.
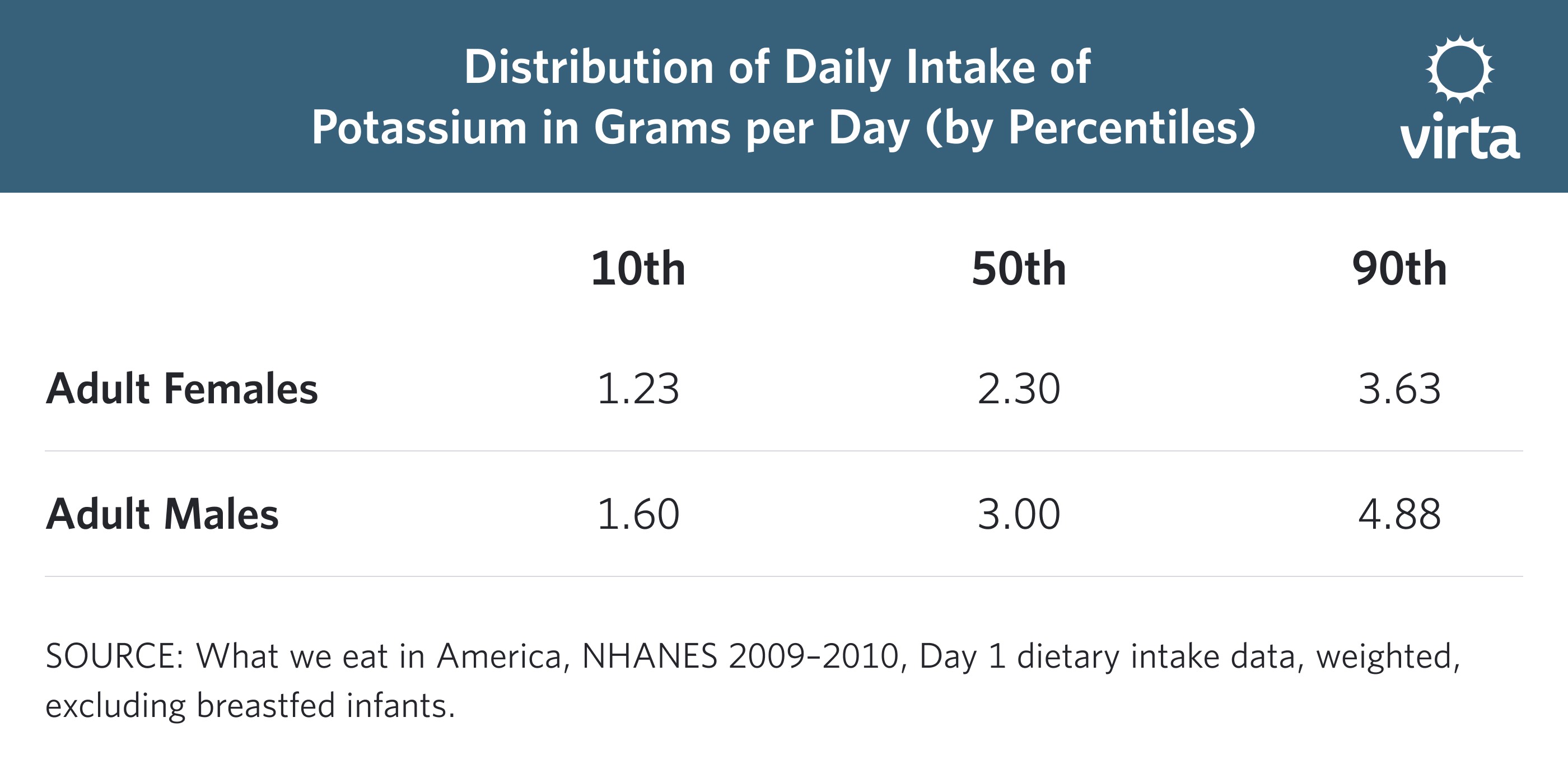
What this shows is that on average, the potassium intake for about half of the population is pretty good; but at the lower end of the diet spectrum people are down in the worrisome intake range.
The answer to the third and final question—What happens when someone adopts a low carbohydrate diet?—depends on what we can, and choose to, include in that diet. It is instructive to see some of the common sources of potassium in the diet.
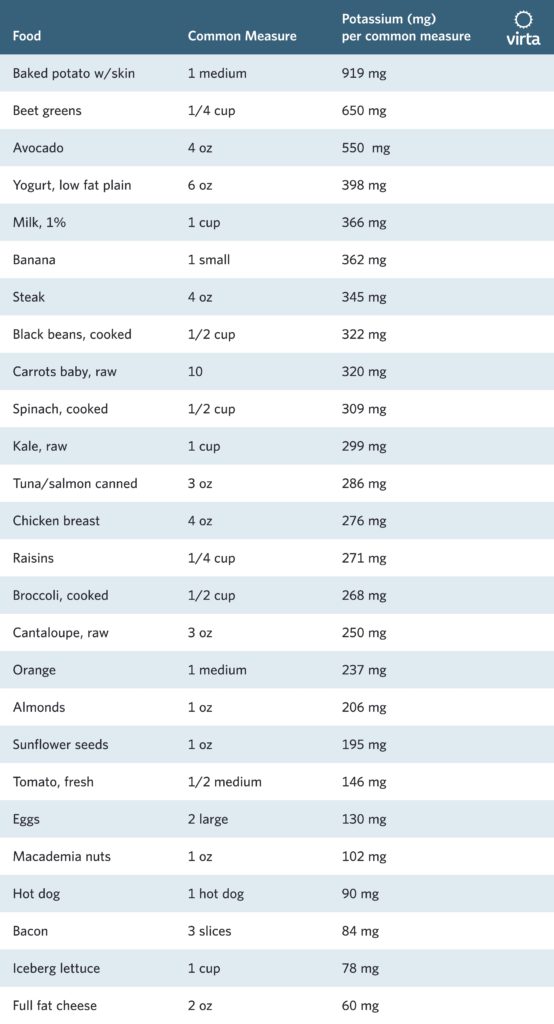
Obviously, when we take away fruit and starchy vegetables, some of the richest sources of this essential electrolyte are off the table (literally!). Second, since protein is consumed in moderation on a well-formulated ketogenic diet, a total of 14-18 ounces of unprocessed meat, fish, or poultry will contribute about 1 gram per day to one’s daily potassium intake. An important point to note here is that processing of meat to create luncheon meat, hot dogs, or bacon removes much of the potassium originally associated with that protein source. Thus, these should be limited as primary protein sources. In addition, if unprocessed protein sources are boiled or stewed, some of the potassium they contain comes out in the broth. Thus they should be prepared and served such that the broth or sauce is consumed to get the full benefit of their electrolytes and minerals.
Official Dietary Potassium Guidelines
How does this information stack up against the official U.S. Recommended Dietary Allowance (RDA)? The surprising answer is that there is no official RDA for potassium. Instead, the last committee to review this topic in 2005 set an ‘Adequate Intake’ value of 4.7 grams per day for adults. Adequate Intake (AI) values are set when there is insufficient evidence to determine an RDA value. The current dietary guidelines committee is reviewing the issue of setting an RDA for potassium, but its report is almost a year overdue. Clearly there is a good deal of uncertainty around defining the ideal dietary potassium intake, particularly since the great majority of the population eats far less than the current AI value of 4.7 grams.
One reason for the confusion in defining optimum dietary potassium values is the close relationship between the regulation of sodium and potassium levels in the body. In general terms (for those interested, more technical detail is provided below), when dietary sodium is restricted, the kidneys tend to excrete more potassium in an attempt to cling to sodium. Thus, sodium restriction increases the need for dietary potassium. This process is regulated by a series of hormones, with the main one being the stress hormone aldosterone. This relationship has been the subject of many clinical studies, and on average a sodium restricted diet given to people with normal blood pressure increases this stress hormone more than 3-fold (5). This is both another reason to avoid sodium restriction if one does not have salt-sensitive high blood pressure, and it is also a good reason to be wary of potassium guidelines that are based upon studies of people following a sodium restricted diet.
Getting Enough Potassium with a Well-Formulated Ketogenic Diet
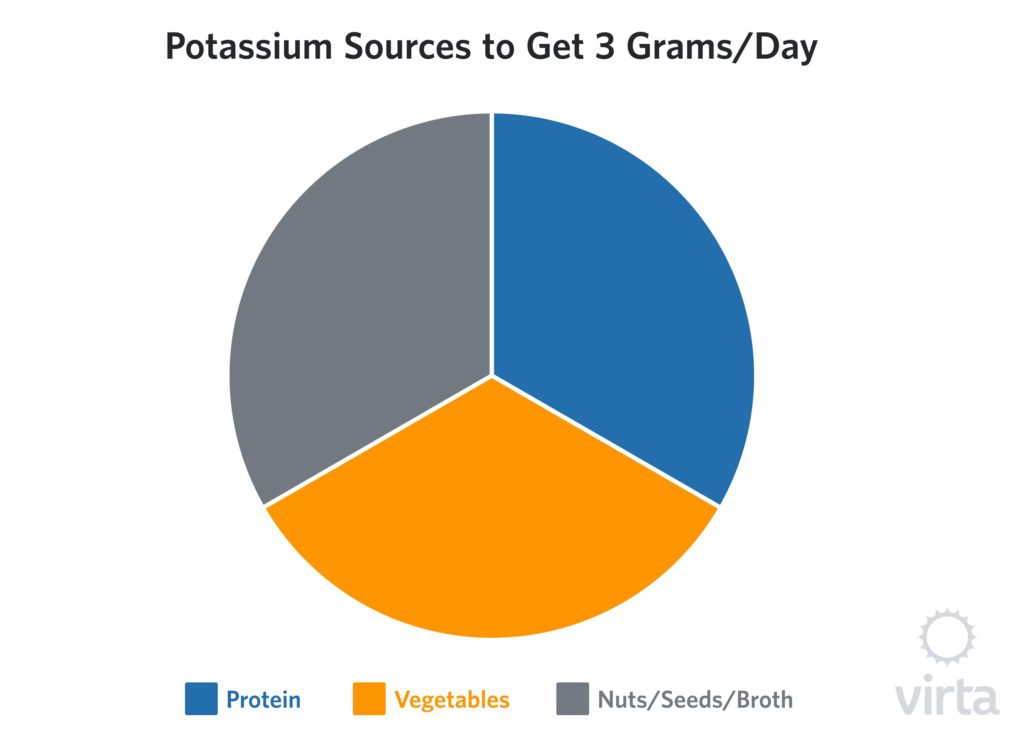
From what we currently know about potassium needs for someone getting adequate sodium on a WFKD, 3 grams per day of potassium (perhaps closer to 4 grams per day), appears to be an appropriate target to provide the necessary amount of potassium for health-related benefits. Also, this is an amount that is credibly achievable with real foods.
To begin, the right choices of protein that are prepared correctly will provide the first gram. On average, non-starchy vegetables that are consumed raw, sautéed or steamed contain about 200 mg per standard serving, so 4-5 servings of vegetables per day will provide the second gram. Nuts and seeds vary in their potassium content but range from 100-300 mg per ounce (oz), so 2 oz per day moves the scale closer to the 3 g per day optimum target.
Broth
The amount of potassium in home-made broth will vary depending upon how much meat remains on the bones used to prepare the broth. Typically, a pound of chicken carcass or meaty beef bones used to make a quart of broth will contain 200-300 mg of potassium per cup. In contrast, most, but not all, commercial ‘bone broths’ and bouillon cubes/granules will vary from 150 down to zero mg of potassium per cup, so seek out those with a higher potassium content.
A Brief Digression: A Classic Science Error Resulting from Ignoring the Broth
In our chapter on ‘Research Pitfalls’ in the Art and Science of Low Carbohydrate Living (6), we critiqued a commonly cited 1980 study by a highly regarded research group (7) that compared two very low calorie diets (about 450 kcal each)—one composed of just boiled turkey and the other consisting of half turkey and half grape juice. For the turkey only, they assumed that most of their potassium intake was coming from the meat, whereas in the other group the potassium intakes came about equally from the meat and grape juice. In both cases, the boiled meat was served and the broth discarded; but unbeknownst to these scientists, they were tossing out about half of the potassium that was originally in the meat. As a result, the protein-only group was receiving much less potassium than expected. An additional problem was that the sodium intakes with both these diets were very restricted, but the higher ketone levels of the protein-only group predictably caused greater sodium losses (aka, the ‘natriuresis of fasting [described below]). This in turn caused the kidneys to try to retain sodium at the expense of potassium through the actions of the hormone aldosterone. However, the researchers incorrectly blamed the symptomatic low blood pressure and greater weakness in the protein-only group on the lack of dietary carbohydrate, ignoring the fact that they had deprived these patients of adequate potassium and sodium intakes.
Lite Salt™: a Backup Electrolyte Insurance Policy
Although whole foods are always the preferred way to obtain these nutrients, at times when that is impractical due to cost or availability, a product like Morton’s Lite Salt is a viable option. This product contains a mixture of sodium chloride and potassium chloride (290mg and 350mg per ¼ tsp, respectively) and can be used to ensure that electrolyte needs are met. For example, a half teaspoon of this mixture added to food or to either commercial or homemade broth can boost daily potassium intake by 0.7 grams, while at the same time adding a modest amount of sodium as well.

Potassium Supplements
By federal statute, non-prescription potassium supplements are limited to 99 mg per dose. These come in a variety of forms such as potassium chloride, succinate, and gluconate. They typically cost 5 cents or more per pill, which translates to about 50 cents per gram of potassium (i.e., the content from ten 99 mg pills). In contrast to this, an 11 oz container of Lite Salt or comparable product costs $4 and provides a gram of potassium for about 5 cents. (Please note that if you are on medications for blood pressure, heart, or kidney problems, it is advised that you consult with a clinician prior to using over-the-counter potassium supplements.)
Technical Information on the Regulation of Electrolyte Balance
It is known that both total fasting and a ketogenic diet lead to an accelerated sodium excretion that increases water and salt loss through the urine. This is known as the natriuresis of fasting. If this lost sodium is not replaced, the resulting deficit sounds off the alarm telling the body to conserve this vital element. The kidneys will reabsorb sodium to reduce its excretion, and though effective at conserving sodium, this process comes at the price of increased potassium excretion. Consistent loss of potassium and/or chronically low intake of potassium can result in a sub-clinical potassium deficiency that the body will attempt to correct via the release of intracellular potassium from skeletal muscle (8). This enables plasma levels to remain “normal” but at a significant consequence to skeletal muscle preservation and function.
It is clear that maintaining sufficient sodium and potassium intakes from the diet serves a number of important functions: potential mitigation of risk for cardiac events, preservation of plasma volume and muscle mass, prevention or reduction of symptoms of the ‘keto- flu,’ as well as a reduction in the unnecessary activation of the hormonal system responsible for the regulation of sodium-potassium balance.
The fail-safe endocrine system responsible for the tight regulation of electrolytes is commonly referred to as the renin-angiotensin-aldosterone system (RAAS). When plasma sodium levels are low (an intake of less than 3 grams per day), when blood potassium levels are significantly elevated (hyperkalemia), or when there is a notable reduction in blood pressure, RAAS is activated in an effort to effectively correct these potentially threatening conditions. While this system does try to keep electrolytes largely in balance, just like any insurance, it comes at a price. RAAS is there when you need it for emergencies but if you use it too much, the price you pay goes up. The cost for frequent RAAS activation is increased oxidative stress, increased vascular damage, measurable dyslipidemia and potential sleep and mood disturbances (9–13). This occurs because many of the conditions that cause RAAS activation, like low sodium levels, are perceived as stressors by the body.
This compensatory activity of RAAS as well as increased sympathetic nervous system activity (14) that together work to maintain electrolyte levels helps explain why we typically do not see a large decrease in blood pressure when sodium is restricted in most patients. In those who do not have salt-sensitive hypertension, these systems appear to adjust to dietary intake and manipulate sodium, potassium and fluid levels in order to maintain a person’s blood pressure.
If the cardioprotective effects of potassium weren’t enough, the important role of potassium in muscle function and sodium in maintaining plasma volume are added considerations for individuals who exercise or engage in activity that results in a large volume of sweat loss. Due to the loss of Na+ and K+ in sweat, these circumstances may require additional electrolyte replacement in order to maintain performance, especially for those following a ketogenic way of eating. A good rule of thumb is about ½ tsp of salt 30 minutes prior to exercise and if exercise is performed at a relatively-high intensity in a hot environment, an additional ½ tsp of salt each hour may be warranted.
Wrap-up
There are a variety of reasons why individuals choose to follow a ketogenic diet, but the common thread is generally a desire for better health and well-being. To achieve the best results, we have previously described the tenets of a well-formulated ketogenic diet that includes advice to get “enough electrolytes and intercellular minerals to maintain optimum circulatory, muscle, and nerve functions.” Consuming the recommended amounts of these electrolytes on daily basis (Na+ 3-5 g and K+ 3-4 g per day) will help support overall health as well as the success and sustainability of nutritional ketosis, regardless of your goals.
A note of caution: If you are taking a diuretic medication (aka, a water pill), if you have high blood pressure, if you have any impairment in kidney function, or if you have limited heart function (such as congestive heart failure), talk to your doctor about your sodium and potassium needs.
The information we provide at virtahealth.com and blog.virtahealth.com is not medical advice, nor is it intended to replace a consultation with a medical professional. Please inform your physician of any changes you make to your diet or lifestyle and discuss these changes with them. If you have questions or concerns about any medical conditions you may have, please contact your physician.
This blog is intended for informational purposes only and is not meant to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition or any advice relating to your health. View full disclaimer
Are you living with type 2 diabetes, prediabetes, or unwanted weight?

- Mahtani, KR., Heneghan, C., Onakpoya, I., et al. Reduced Salt Intake for Heart Failure: A Systematic Review. JAMA Intern Med. 2018; E1-E7
- Yang, Q., Liu, T., Kuklina, EV., et al. Sodium and Potassium Intake and Mortality Among US Adults Prospective Data From the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2011;171(13):1183-1191
- Leonberg-Yoo AK, Tighiouart H, Levey AS, et al. Urine Potassium Excretion, Kidney Failure, and Mortality in CKD. Am J Kidney Dis. 2017; 69:341-349
- O’Donnell, M., Mente, A., Rangarajan, S., et al. Urinary Sodium and Potassium Excretion, Mortality, and Cardiovascular Events. N Engl J Med. 2014; 371:612-623
- Graudal NA, Galløe AM, Garred P. Effects of Sodium Restriction on Blood Pressure, Renin, Aldosterone, Catecholamines, Cholesterols, and Triglyceride; A Meta-analysis. JAMA. 1998; 279:1383-1391
- Volek, JS., Phinney, SD., The Art and Science of Low Carbohydrate Living. Beyond Obesity, LLC, 2011
- DeHaven, J., Sherwin, R., Hendler, R., et al. Nitrogen and sodium balance and sympathetic-nervous-system activity in obese subjects treated with a low-calorie protein or mixed diet. New Engl J Med. 1980; 302;477-482
- McDonough, AA., Thompson, CB., Youn, JH. Skeletal muscle regulates extracellular potassium. Am J Physiol Renal Physiol. 2002; 282: F967–F974
- Dzau, VJ. Tissue Angiotensin and Pathobiology of Vascular Disease: A Unifying Hypothesis. Hypertension. 2001; 37:1047-1052
- van Thiel, BS., van der Pluijm, I., te Riet, L., et al. The renin–angiotensin system and its involvement in vascular disease. European Journal of Pharmacology. 2015; 763: 3–14
- Graudal, NA., Hubeck-Graudal, T., Jürgens, G. Effects of Low-Sodium Diet vs. High-Sodium Diet on Blood Pressure, Renin, Aldosterone, Catecholamines, Cholesterol, and Triglyceride (Cochrane Review). Am J Hypertension. 2012; 25(1):1-15
- Murck, H., Schüssler, P., Steiger, A. Renin-Angiotensin-Aldosterone System: The Forgotten Stress Hormone System: Relationship to Depression and Sleep. Pharmacopsychiatry. 2012;45:83-95
- Grippo, AJ., Moffitt, JA., Beltz, TG., et al. Reduced Hedonic Behavior and Altered Cardiovascular Function Induced by Mild Sodium Depletion in Rats. Behavioral Neuroscience. 2006; 120(5):1133-1143
- Warren, SE., Vieweg, WVR., O’Connor, DT. Sympathetic Nervous System Activity during Sodium Restriction in Essential Hypertension. Clin Cardiol. 1980; 3:348-351